正在加载图片...
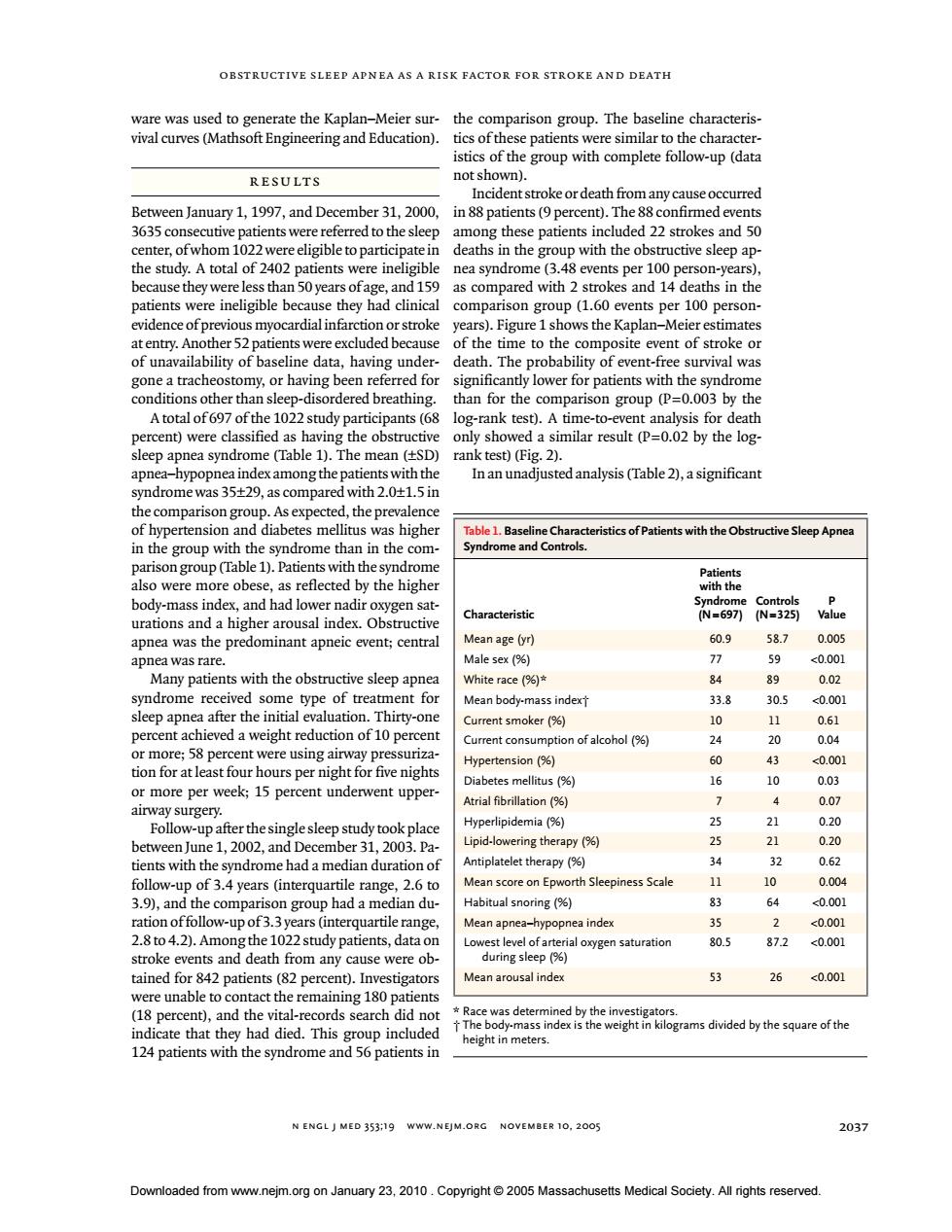
OBSTRUCTIVE SLEEP APNEA AS A RISK FACTOR FOR STROKE AND DEATH ware was used to generate the kaplan-Meier sur-the comparison group.The baseline characteris- vival curves(Mathsoft Engineering and Education).tics ofthese patients were similar to the character- istics of the group with complete follow-up(data resuLts not Between January 1,1997,and December31,2000,in88 patients(9per cent).The confirmed events 335consecutive patients were referredto thesleep among these patients included 22 strokes and50 A tota 50 were ine d wirh 2 s evidence of pre viou years).Figure 1shows the Kaplan-Meier estimates entry.A er 52 e to the omposite e ent or significantly lower fo than for the comparison group (P=0.003 by the )were class by the log- )(Fi apnea hypopnea index among the patients with the In an unadjusted analysis(Table2),a significant yndromewas35+9,as compared with 2.01.in thepr ne than in th ients with the Obstructive Sle n with the th the body-mass nde -697 Mean age (yr) 60.9 58.7 0.005 apnea was rare. Male sex(%) 77 Many patients ith the obstructive White race(%) 0.02 ent fo ean body-mass indexT 33.8 Thi 305 0.00 percent achieved a weight reducion of10 nt smoker (% ent consumption of alcohol ours per nig ctension % 040 12030 trial fibrillati oferthensytook plac pide 0.20 y%) 21 0.20 therapy(% 14 Mean score on Epv rth Sleepiness Scale 10 0.004 Ro)and the co n gr p had a median du Habitual snoring (% 20.01 tion offollow-upof3years ( Mean apnea-hype nea index 2 <0.00 2.8o4.2.Am0 2 study patients,data ial oxygen saturation 80.5 87.2 <0.001 ed fve m any 26 <0.001 were unable to contact the remaining 180 patients 18 percent),and the vital-records search did no had di t N ENGLJ MED 353:19 www.NEjM.ORC NOVEMBER 10,2005 2037 Dowloaded from www.23.010.Massachusetts Medical Socety.All rights reserved. n engl j med 353;19 www.nejm.org november 10, 2005 obstructive sleep apnea as a risk factor for stroke and death 2037 ware was used to generate the Kaplan–Meier survival curves (Mathsoft Engineering and Education). Between January 1, 1997, and December 31, 2000, 3635 consecutive patients were referred to the sleep center, of whom 1022 were eligible to participate in the study. A total of 2402 patients were ineligible because they were less than 50 years of age, and 159 patients were ineligible because they had clinical evidence of previous myocardial infarction or stroke at entry. Another 52 patients were excluded because of unavailability of baseline data, having undergone a tracheostomy, or having been referred for conditions other than sleep-disordered breathing. A total of 697 of the 1022 study participants (68 percent) were classified as having the obstructive sleep apnea syndrome (Table 1). The mean (±SD) apnea–hypopnea index among the patients with the syndrome was 35±29, as compared with 2.0±1.5 in the comparison group. As expected, the prevalence of hypertension and diabetes mellitus was higher in the group with the syndrome than in the comparison group (Table 1). Patients with the syndrome also were more obese, as reflected by the higher body-mass index, and had lower nadir oxygen saturations and a higher arousal index. Obstructive apnea was the predominant apneic event; central apnea was rare. Many patients with the obstructive sleep apnea syndrome received some type of treatment for sleep apnea after the initial evaluation. Thirty-one percent achieved a weight reduction of 10 percent or more; 58 percent were using airway pressurization for at least four hours per night for five nights or more per week; 15 percent underwent upperairway surgery. Follow-up after the single sleep study took place between June 1, 2002, and December 31, 2003. Patients with the syndrome had a median duration of follow-up of 3.4 years (interquartile range, 2.6 to 3.9), and the comparison group had a median duration of follow-up of 3.3 years (interquartile range, 2.8 to 4.2). Among the 1022 study patients, data on stroke events and death from any cause were obtained for 842 patients (82 percent). Investigators were unable to contact the remaining 180 patients (18 percent), and the vital-records search did not indicate that they had died. This group included 124 patients with the syndrome and 56 patients in the comparison group. The baseline characteristics of these patients were similar to the characteristics of the group with complete follow-up (data not shown). Incident stroke or death from any cause occurred in 88 patients (9 percent). The 88 confirmed events among these patients included 22 strokes and 50 deaths in the group with the obstructive sleep apnea syndrome (3.48 events per 100 person-years), as compared with 2 strokes and 14 deaths in the comparison group (1.60 events per 100 personyears). Figure 1 shows the Kaplan–Meier estimates of the time to the composite event of stroke or death. The probability of event-free survival was significantly lower for patients with the syndrome than for the comparison group (P=0.003 by the log-rank test). A time-to-event analysis for death only showed a similar result (P=0.02 by the logrank test) (Fig. 2). In an unadjusted analysis (Table 2), a significant results * Race was determined by the investigators. † The body-mass index is the weight in kilograms divided by the square of the height in meters. Table 1. Baseline Characteristics of Patients with the Obstructive Sleep Apnea Syndrome and Controls. Characteristic Patients with the Syndrome (N=697) Controls (N=325) P Value Mean age (yr) 60.9 58.7 0.005 Male sex (%) 77 59 <0.001 White race (%)* 84 89 0.02 Mean body-mass index† 33.8 30.5 <0.001 Current smoker (%) 10 11 0.61 Current consumption of alcohol (%) 24 20 0.04 Hypertension (%) 60 43 <0.001 Diabetes mellitus (%) 16 10 0.03 Atrial fibrillation (%) 7 4 0.07 Hyperlipidemia (%) 25 21 0.20 Lipid-lowering therapy (%) 25 21 0.20 Antiplatelet therapy (%) 34 32 0.62 Mean score on Epworth Sleepiness Scale 11 10 0.004 Habitual snoring (%) 83 64 <0.001 Mean apnea–hypopnea index 35 2 <0.001 Lowest level of arterial oxygen saturation during sleep (%) 80.5 87.2 <0.001 Mean arousal index 53 26 <0.001 Downloaded from www.nejm.org on January 23, 2010 . Copyright © 2005 Massachusetts Medical Society. All rights reserved