正在加载图片...
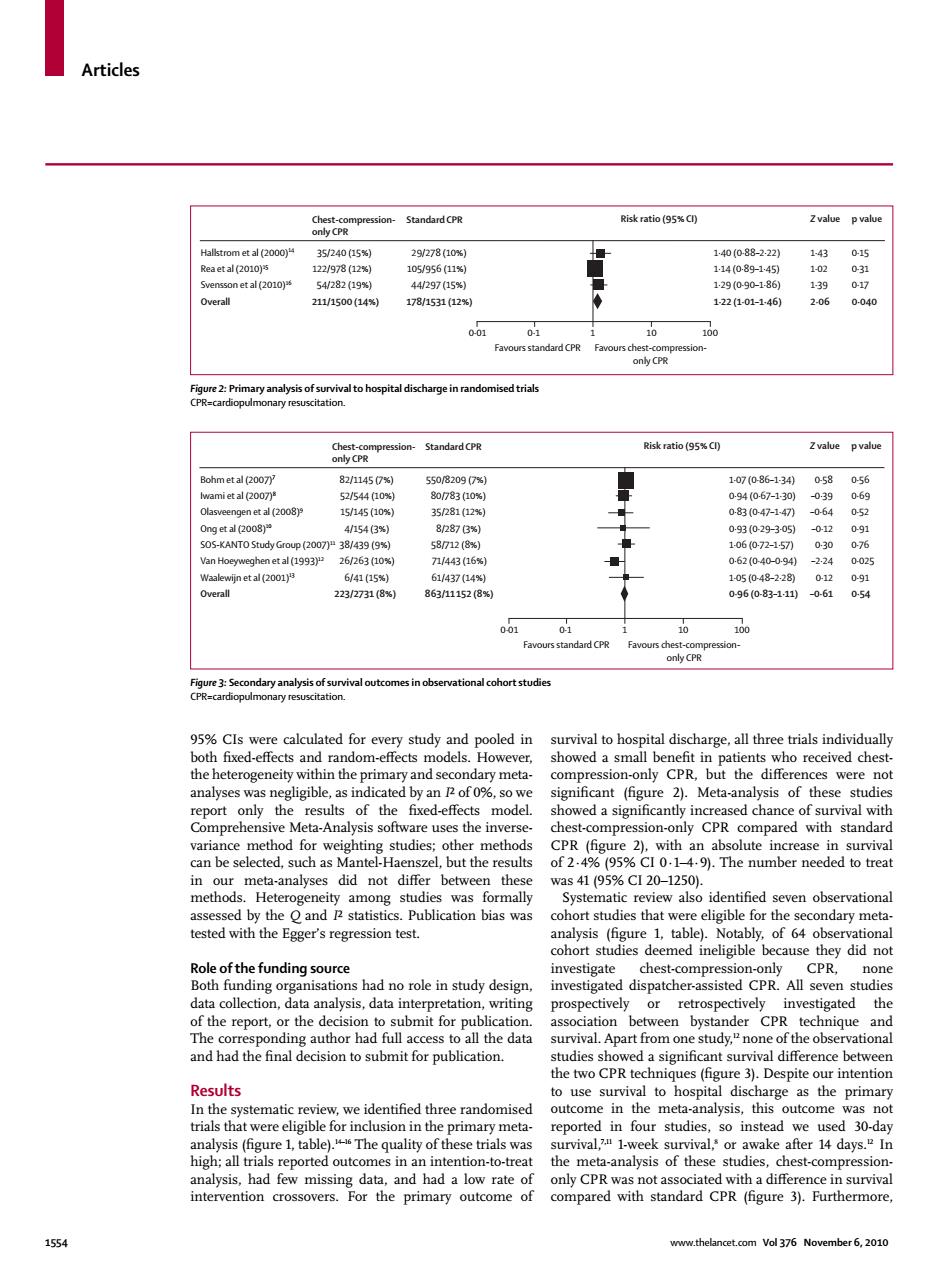
Articles Risk ratio (95%C) OGg中 sand山rd cPR Zvalue pvalue et al 2000 5240(a5% 298(ao 2111500(14 178/153112% 122101-140 004 tandard CPR only CPR ession Standard CPR Risk ratio (95%Cl) td2007 2/1457) 1(2008 15/145 (10 282 3/231(8 11152(8 100 ional cohort 5%CIs w ecalculated for every study and pooled in survival to hospital discharge,all three trials individually the hete ithinthe prima a sm analyses v igificant (figure 2).Meta-ana ysis of these studie ared with standard van l but th n our m thes 254195%C20-1250 E tested with the Egger's regression test. CPR on ions had no role in study design. submit for he two CPR techi es Despite our intentior Results In the utcome in the me analysis.this outcome not trials tha ere elig or inclusion in th our studie entionto-re meta-analysis of thes hest-comp compared with standard. n Vol 376 November 6.2010 Articles 1554 www.thelancet.com Vol 376 November 6, 2010 95% CIs were calculated for every study and pooled in both fi xed-eff ects and random-eff ects models. However, the heterogeneity within the primary and secondary metaanalyses was negligible, as indicated by an I² of 0%, so we report only the results of the fi xed-eff ects model. Comprehensive Meta-Analysis software uses the inversevariance method for weighting studies; other methods can be selected, such as Mantel-Haenszel, but the results in our meta-analyses did not diff er between these methods. Heterogeneity among studies was formally assessed by the Q and I² statistics. Publication bias was tested with the Egger’s regression test. Role of the funding source Both funding organisations had no role in study design, data collection, data analysis, data interpretation, writing of the report, or the decision to submit for publication. The corresponding author had full access to all the data and had the fi nal decision to submit for publication. Results In the systematic review, we identifi ed three randomised trials that were eligible for inclusion in the primary metaanalysis (fi gure 1, table).14–16 The quality of these trials was high; all trials reported outcomes in an intention-to-treat analysis, had few missing data, and had a low rate of intervention crossovers. For the primary outcome of survival to hospital discharge, all three trials individually showed a small benefi t in patients who received chestcompression-only CPR, but the diff erences were not signifi cant (fi gure 2). Meta-analysis of these studies showed a signifi cantly increased chance of survival with chest-compression-only CPR compared with standard CPR (fi gure 2), with an absolute increase in survival of 2·4% (95% CI 0·1–4·9). The number needed to treat was 41 (95% CI 20–1250). Systematic review also identifi ed seven observational cohort studies that were eligible for the secondary metaanalysis (fi gure 1, table). Notably, of 64 observational cohort studies deemed ineligible because they did not investigate chest-compression-only CPR, none investigated dispatcher-assisted CPR. All seven studies prospectively or retrospectively investigated the association between bystander CPR technique and survival. Apart from one study,12 none of the observational studies showed a signifi cant survival diff erence between the two CPR techniques (fi gure 3). Despite our intention to use survival to hospital discharge as the primary outcome in the meta-analysis, this outcome was not reported in four studies, so instead we used 30-day survival,7,11 1-week survival,8 or awake after 14 days.12 In the meta-analysis of these studies, chest-compressiononly CPR was not associated with a diff erence in survival compared with standard CPR (fi gure 3). Furthermore, Figure 2: Primary analysis of survival to hospital discharge in randomised trials CPR=cardiopulmonary resuscitation. 0·15 0·31 0·17 0·040 1·43 1·02 1·39 2·06 1·40 (0·88–2·22) 1·14 (0·89–1·45) 1·29 (0·90–1·86) 1·22 (1·01–1·46) 35/240 (15%) 122/978 (12%) 54/282 (19%) 211/1500 (14%) 29/278 (10%) 105/956 (11%) 44/297 (15%) 178/1531 (12%) Chest-compressiononly CPR Standard CPR Hallstrom et al (2000)14 Rea et al (2010)15 Svensson et al (2010)16 Overall Risk ratio (95% CI) Z value p value Favours standard CPR Favours chest-compressiononly CPR 0·01 0·1 1 10 100 0·56 0·69 0·52 0·91 0·76 0·025 0·91 0·54 0·58 –0·39 –0·64 –0·12 0·30 –2·24 0·12 –0·61 1·07 (0·86–1·34) 0·94 (0·67–1·30) 0·83 (0·47–1·47) 0·93 (0·29–3·05) 1·06 (0·72–1·57) 0·62 (0·40–0·94) 1·05 (0·48–2·28) 0·96 (0·83–1·11) 82/1145 (7%) 52/544 (10%) 15/145 (10%) 4/154 (3%) 38/439 (9%) 26/263 (10%) 6/41 (15%) 223/2731 (8%) 550/8209 (7%) 80/783 (10%) 35/281 (12%) 8/287 (3%) 58/712 (8%) 71/443 (16%) 61/437 (14%) 863/11152 (8%) Chest-compressiononly CPR Standard CPR Bohm et al (2007)7 Iwami et al (2007)8 Olasveengen et al (2008)9 Ong et al (2008)10 SOS-KANTO Study Group (2007)11 Van Hoeyweghen et al (1993)12 Waalewijn et al (2001)13 Overall Risk ratio (95% CI) Z value p value Favours standard CPR Favours chest-compressiononly CPR 0·01 0·1 1 10 100 Figure 3: Secondary analysis of survival outcomes in observational cohort studies CPR=cardiopulmonary resuscitation