正在加载图片...
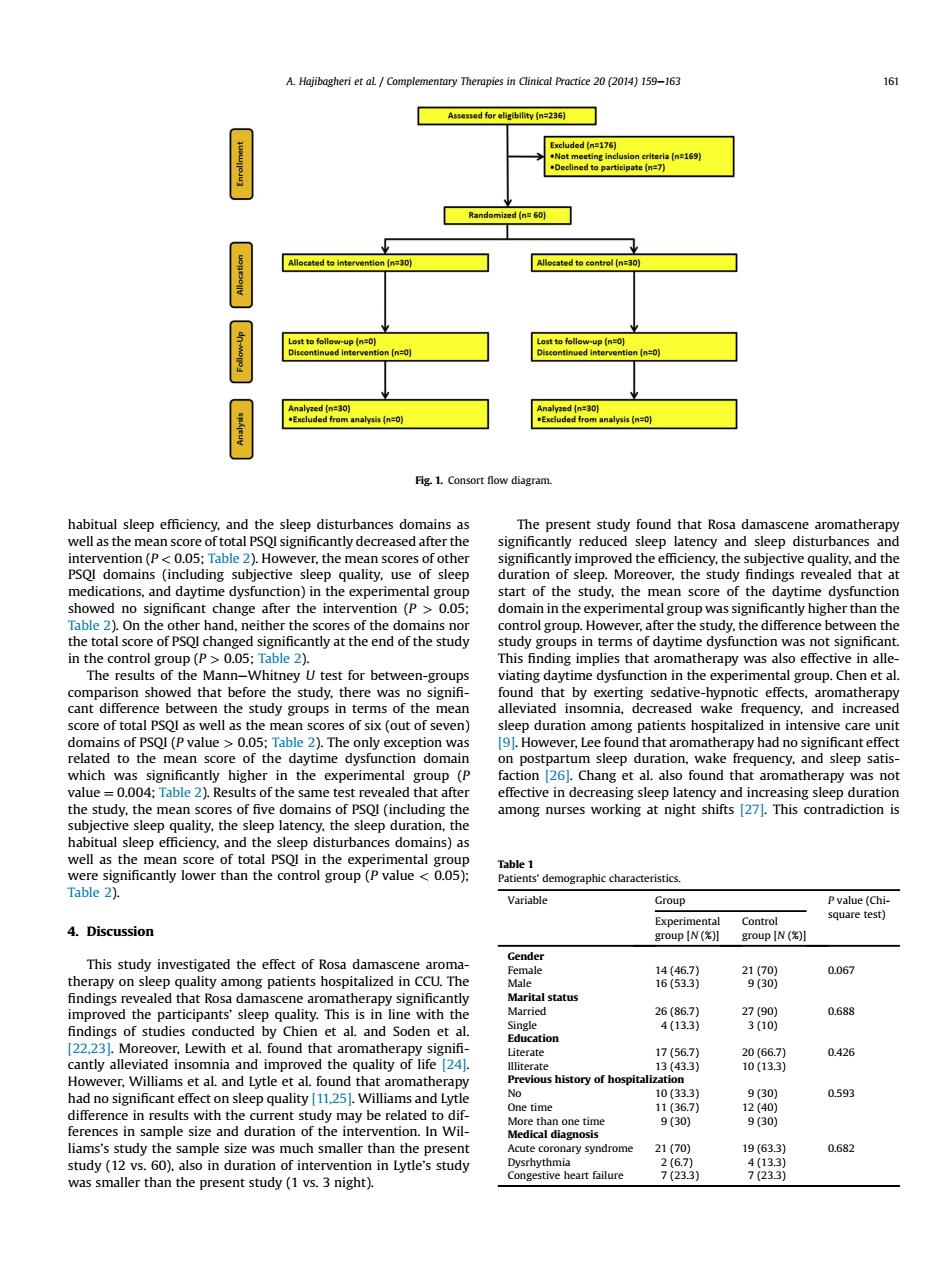
A.Hajibagheri et aL Complementary Therapies in Clinical Practice 20(2014)159-163 161 Assessed for eligibllity (n=236) Excluded (n=176) ng in ria(n=169 .Declined to participate (n=7) Randomized (n=60) cated to int Allocated to contr Analyzed (n=30) Analyzed (n=30) .Excluded from analysis (n=0) .Excluded from analysis (n=0) Fig.1.Consort flow diagram. habitual sleep efficiency.and the sleep disturbances domains as The present study found that Rosa damascene aromatherapy well as the mean score of total PSQI significantly decreased after the significantly reduced sleep latency and sleep disturbances and intervention(P<0.05;Table 2).However,the mean scores of other significantly improved the efficiency,the subjective quality,and the PSQI domains (including subjective sleep quality.use of sleep duration of sleep.Moreover,the study findings revealed that at medications,and daytime dysfunction)in the experimental group start of the study,the mean score of the daytime dysfunction showed no significant change after the intervention (P>0.05; domain in the experimental group was significantly higher than the Table 2).On the other hand,neither the scores of the domains nor control group.However,after the study,the difference between the the total score of PSQl changed significantly at the end of the study study groups in terms of daytime dysfunction was not significant in the control group (P >0.05;Table 2). This finding implies that aromatherapy was also effective in alle- The results of the Mann-Whitney U test for between-groups viating daytime dysfunction in the experimental group.Chen et al. comparison showed that before the study,there was no signifi- found that by exerting sedative-hypnotic effects,aromatherapy cant difference between the study groups in terms of the mean alleviated insomnia,decreased wake frequency,and increased score of total PSQI as well as the mean scores of six (out of seven) sleep duration among patients hospitalized in intensive care unit domains of PSQI(P value >0.05;Table 2).The only exception was [9].However,Lee found that aromatherapy had no significant effect related to the mean score of the daytime dysfunction domain on postpartum sleep duration,wake frequency,and sleep satis- which was significantly higher in the experimental group (P faction [26].Chang et al.also found that aromatherapy was not value =0.004;Table 2).Results of the same test revealed that after effective in decreasing sleep latency and increasing sleep duration the study,the mean scores of five domains of PSQl (including the among nurses working at night shifts [27.This contradiction is subjective sleep quality,the sleep latency,the sleep duration,the habitual sleep efficiency,and the sleep disturbances domains)as well as the mean score of total PSQl in the experimental group Table 1 were significantly lower than the control group (P value 0.05): Patients'demographic characteristics. Table 2). Variable Group P value (Chi- Experimental Control square test) 4.Discussion group [N () group [N () Gender This study investigated the effect of Rosa damascene aroma Female 14(46.7) 21(70) 0.067 therapy on sleep quality among patients hospitalized in CCU.The Male 16(53.3) 9(30) findings revealed that Rosa damascene aromatherapy significantly Marital status improved the participants'sleep quality.This is in line with the Married 26(86.7) 27(90) 0.688 findings of studies conducted by Chien et al.and Soden et al. Single 4(13.3) 3(10) Education [22.23].Moreover,Lewith et al found that aromatherapy signifi- Literate 17(56.7) 20(66.7) 0.426 cantly alleviated insomnia and improved the quality of life [24]. llliterate 13(43.3) 10(133) However,Williams et al.and Lytle et al.found that aromatherapy Previous history of hospitalization had no significant effect on sleep quality [11.25].Williams and Lytle No 10(33.3) 9(30) 0.593 One time 11(36.7) 12(40) difference in results with the current study may be related to dif- More than one time 9(30) 9(30) ferences in sample size and duration of the intervention.In Wil- Medical diagnosis liams's study the sample size was much smaller than the present Acute coronary syndrome 21(70) 19(633) 0.682 study (12 vs.60),also in duration of intervention in Lytle's study Dysrhythmia 2(6.7) 4(133) was smaller than the present study(1 vs.3 night). Congestive heart failure 7(233) 7(23.3)habitual sleep efficiency, and the sleep disturbances domains as well as the mean score of total PSQI significantly decreased after the intervention (P < 0.05; Table 2). However, the mean scores of other PSQI domains (including subjective sleep quality, use of sleep medications, and daytime dysfunction) in the experimental group showed no significant change after the intervention (P > 0.05; Table 2). On the other hand, neither the scores of the domains nor the total score of PSQI changed significantly at the end of the study in the control group (P > 0.05; Table 2). The results of the ManneWhitney U test for between-groups comparison showed that before the study, there was no signifi- cant difference between the study groups in terms of the mean score of total PSQI as well as the mean scores of six (out of seven) domains of PSQI (P value > 0.05; Table 2). The only exception was related to the mean score of the daytime dysfunction domain which was significantly higher in the experimental group (P value ¼ 0.004; Table 2). Results of the same test revealed that after the study, the mean scores of five domains of PSQI (including the subjective sleep quality, the sleep latency, the sleep duration, the habitual sleep efficiency, and the sleep disturbances domains) as well as the mean score of total PSQI in the experimental group were significantly lower than the control group (P value < 0.05); Table 2). 4. Discussion This study investigated the effect of Rosa damascene aromatherapy on sleep quality among patients hospitalized in CCU. The findings revealed that Rosa damascene aromatherapy significantly improved the participants’ sleep quality. This is in line with the findings of studies conducted by Chien et al. and Soden et al. [22,23]. Moreover, Lewith et al. found that aromatherapy signifi- cantly alleviated insomnia and improved the quality of life [24]. However, Williams et al. and Lytle et al. found that aromatherapy had no significant effect on sleep quality [11,25]. Williams and Lytle difference in results with the current study may be related to differences in sample size and duration of the intervention. In Williams’s study the sample size was much smaller than the present study (12 vs. 60), also in duration of intervention in Lytle’s study was smaller than the present study (1 vs. 3 night). The present study found that Rosa damascene aromatherapy significantly reduced sleep latency and sleep disturbances and significantly improved the efficiency, the subjective quality, and the duration of sleep. Moreover, the study findings revealed that at start of the study, the mean score of the daytime dysfunction domain in the experimental group was significantly higher than the control group. However, after the study, the difference between the study groups in terms of daytime dysfunction was not significant. This finding implies that aromatherapy was also effective in alleviating daytime dysfunction in the experimental group. Chen et al. found that by exerting sedative-hypnotic effects, aromatherapy alleviated insomnia, decreased wake frequency, and increased sleep duration among patients hospitalized in intensive care unit [9]. However, Lee found that aromatherapy had no significant effect on postpartum sleep duration, wake frequency, and sleep satisfaction [26]. Chang et al. also found that aromatherapy was not effective in decreasing sleep latency and increasing sleep duration among nurses working at night shifts [27]. This contradiction is Fig. 1. Consort flow diagram. Table 1 Patients’ demographic characteristics. Variable Group P value (Chisquare test) Experimental group [N (%)] Control group [N (%)] Gender Female 14 (46.7) 21 (70) 0.067 Male 16 (53.3) 9 (30) Marital status Married 26 (86.7) 27 (90) 0.688 Single 4 (13.3) 3 (10) Education Literate 17 (56.7) 20 (66.7) 0.426 Illiterate 13 (43.3) 10 (13.3) Previous history of hospitalization No 10 (33.3) 9 (30) 0.593 One time 11 (36.7) 12 (40) More than one time 9 (30) 9 (30) Medical diagnosis Acute coronary syndrome 21 (70) 19 (63.3) 0.682 Dysrhythmia 2 (6.7) 4 (13.3) Congestive heart failure 7 (23.3) 7 (23.3) A. Hajibagheri et al. / Complementary Therapies in Clinical Practice 20 (2014) 159e163 161