正在加载图片...
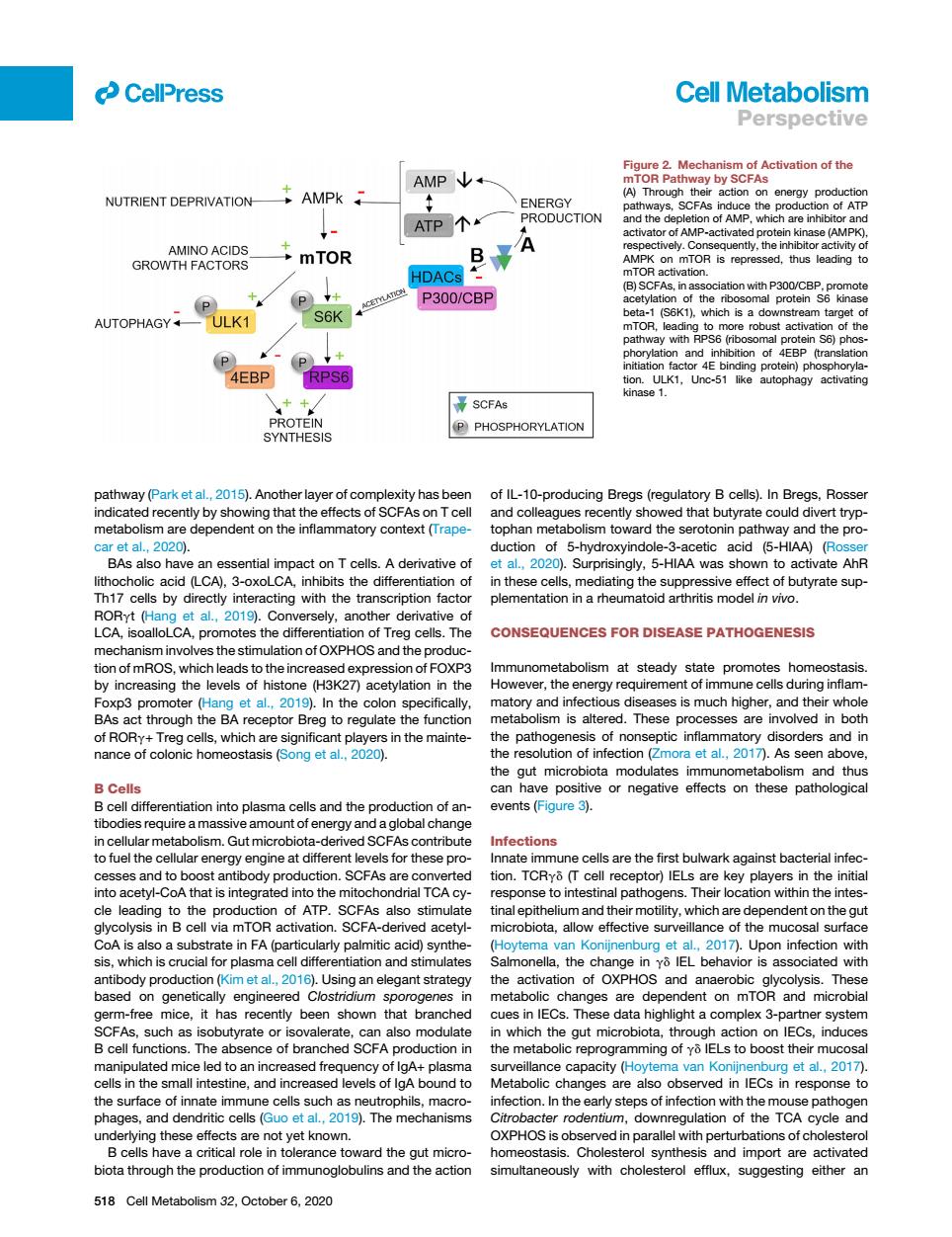
CellPress Cell Metabolism Perspective AMP↓+ NUTRIENT DEPRIVATION AMPK PRODUCTION ce the ATP个 are in mTOR BA R is rep d,thus leading CFAS.in ⊙ P300/CBP of the AUTOPHAGY ULK1 B E act P 4EBP 点 (P PHOSPHORYLATION pathway(Park et al.2015).Another laver of complexity has beer of IL-10-producing Breas (regulatory B cells).In Breas,Rosse and col eagues recenty sho ed that butyrate could divert tryp at al 2020) ction of 5-hydroxyindole-aceiccd As oha entia mpact onT ta,20 0).Surprisingly.5-HIAA was shown to activate AhF Th17cells by directly interacting with the transcription facto plementation in a rheumatoid arthritis model in vivo. yt (H Co rsely,ano den CONSEQUENCES FOR DISEASE PATHOGENESIS mechanism involves the stimulation of OXPHOS and the increa mmun the ene et al.. 2019).In the colon specifically matory and infect diseases is much higher,and th whole recepto eg to reguat nanceof ers and in the(.) As seen above B Cells can have positive or negative effects on these pathological ntiation into plasma cels and the events(Figure 3). Infections o fuel the Gellareneryengneatdtierer se pro drial TC eto intestinal pathogens.Their cation within the intes. production of ATP SCFAs alsc which are ependent on the gu A is also a substrate in FA(parti acid)s 7).Upon infectior tad ce and e in ass sed on genetic are de dent on mTORn micr bial ghlight a co h cell functions.Th n in creprogramming ofs to boost the olic changes the surface of innate imr e cells uch as r nfection.In the early steps of inf on with the n pathoger in tolerance to and import activated ction of immunogl 518 Cell Metabolism 2,October6,020pathway (Park et al., 2015). Another layer of complexity has been indicated recently by showing that the effects of SCFAs on T cell metabolism are dependent on the inflammatory context (Trapecar et al., 2020). BAs also have an essential impact on T cells. A derivative of lithocholic acid (LCA), 3-oxoLCA, inhibits the differentiation of Th17 cells by directly interacting with the transcription factor RORgt (Hang et al., 2019). Conversely, another derivative of LCA, isoalloLCA, promotes the differentiation of Treg cells. The mechanism involves the stimulation of OXPHOS and the production of mROS, which leads to the increased expression of FOXP3 by increasing the levels of histone (H3K27) acetylation in the Foxp3 promoter (Hang et al., 2019). In the colon specifically, BAs act through the BA receptor Breg to regulate the function of RORg+ Treg cells, which are significant players in the maintenance of colonic homeostasis (Song et al., 2020). B Cells B cell differentiation into plasma cells and the production of antibodies require a massive amount of energy and a global change in cellular metabolism. Gut microbiota-derived SCFAs contribute to fuel the cellular energy engine at different levels for these processes and to boost antibody production. SCFAs are converted into acetyl-CoA that is integrated into the mitochondrial TCA cycle leading to the production of ATP. SCFAs also stimulate glycolysis in B cell via mTOR activation. SCFA-derived acetylCoA is also a substrate in FA (particularly palmitic acid) synthesis, which is crucial for plasma cell differentiation and stimulates antibody production (Kim et al., 2016). Using an elegant strategy based on genetically engineered Clostridium sporogenes in germ-free mice, it has recently been shown that branched SCFAs, such as isobutyrate or isovalerate, can also modulate B cell functions. The absence of branched SCFA production in manipulated mice led to an increased frequency of IgA+ plasma cells in the small intestine, and increased levels of IgA bound to the surface of innate immune cells such as neutrophils, macrophages, and dendritic cells (Guo et al., 2019). The mechanisms underlying these effects are not yet known. B cells have a critical role in tolerance toward the gut microbiota through the production of immunoglobulins and the action of IL-10-producing Bregs (regulatory B cells). In Bregs, Rosser and colleagues recently showed that butyrate could divert tryptophan metabolism toward the serotonin pathway and the production of 5-hydroxyindole-3-acetic acid (5-HIAA) (Rosser et al., 2020). Surprisingly, 5-HIAA was shown to activate AhR in these cells, mediating the suppressive effect of butyrate supplementation in a rheumatoid arthritis model in vivo. CONSEQUENCES FOR DISEASE PATHOGENESIS Immunometabolism at steady state promotes homeostasis. However, the energy requirement of immune cells during inflammatory and infectious diseases is much higher, and their whole metabolism is altered. These processes are involved in both the pathogenesis of nonseptic inflammatory disorders and in the resolution of infection (Zmora et al., 2017). As seen above, the gut microbiota modulates immunometabolism and thus can have positive or negative effects on these pathological events (Figure 3). Infections Innate immune cells are the first bulwark against bacterial infection. TCRgd (T cell receptor) IELs are key players in the initial response to intestinal pathogens. Their location within the intestinal epithelium and their motility, which are dependent on the gut microbiota, allow effective surveillance of the mucosal surface (Hoytema van Konijnenburg et al., 2017). Upon infection with Salmonella, the change in gd IEL behavior is associated with the activation of OXPHOS and anaerobic glycolysis. These metabolic changes are dependent on mTOR and microbial cues in IECs. These data highlight a complex 3-partner system in which the gut microbiota, through action on IECs, induces the metabolic reprogramming of gd IELs to boost their mucosal surveillance capacity (Hoytema van Konijnenburg et al., 2017). Metabolic changes are also observed in IECs in response to infection. In the early steps of infection with the mouse pathogen Citrobacter rodentium, downregulation of the TCA cycle and OXPHOS is observed in parallel with perturbations of cholesterol homeostasis. Cholesterol synthesis and import are activated simultaneously with cholesterol efflux, suggesting either an Figure 2. Mechanism of Activation of the mTOR Pathway by SCFAs (A) Through their action on energy production pathways, SCFAs induce the production of ATP and the depletion of AMP, which are inhibitor and activator of AMP-activated protein kinase (AMPK), respectively. Consequently, the inhibitor activity of AMPK on mTOR is repressed, thus leading to mTOR activation. (B) SCFAs, in association with P300/CBP, promote acetylation of the ribosomal protein S6 kinase beta-1 (S6K1), which is a downstream target of mTOR, leading to more robust activation of the pathway with RPS6 (ribosomal protein S6) phosphorylation and inhibition of 4EBP (translation initiation factor 4E binding protein) phosphorylation. ULK1, Unc-51 like autophagy activating kinase 1. ll 518 Cell Metabolism 32, October 6, 2020 Perspective