正在加载图片...
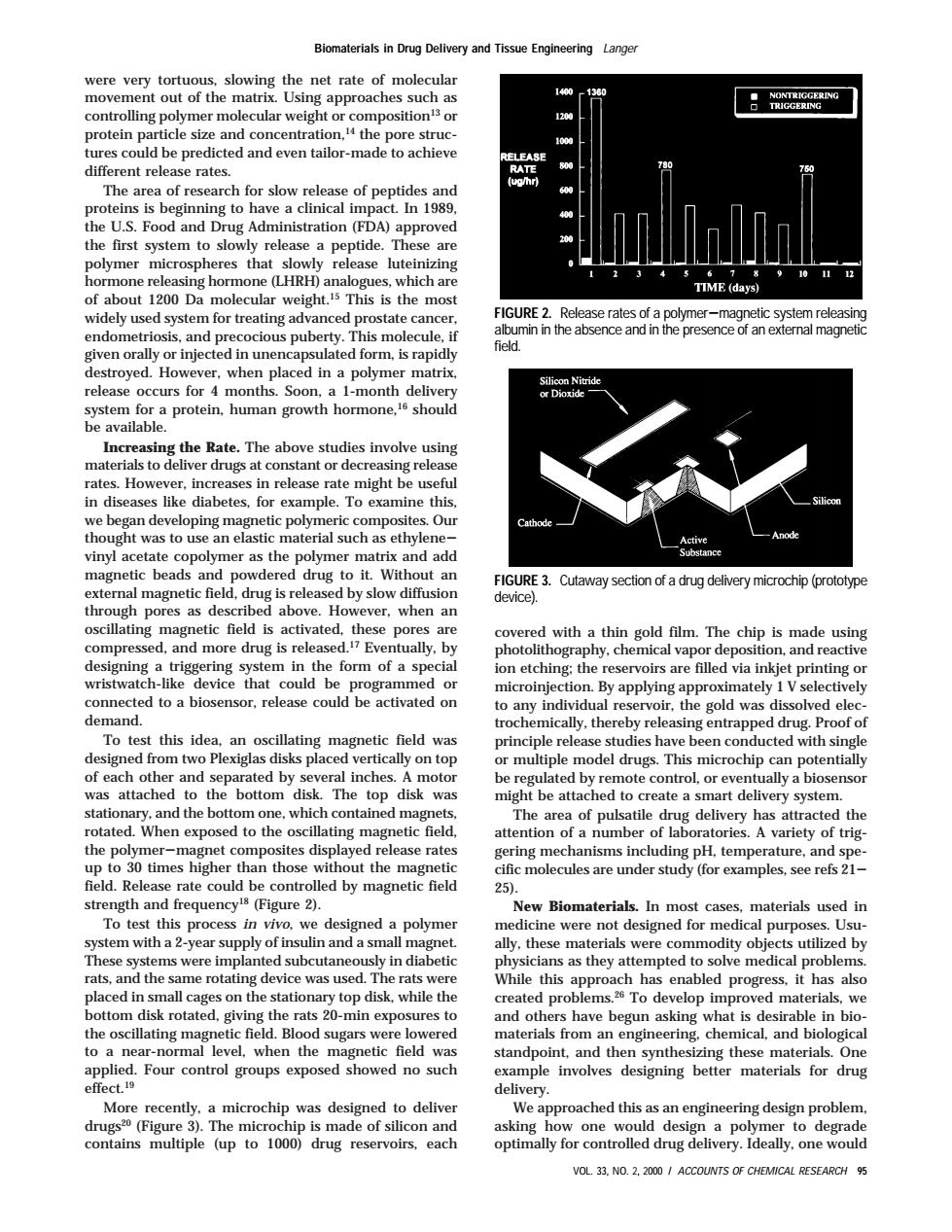
Blomaterials in Drug Delivery and Tissue protein ticle size and concentration,the pore struc cted and even tailor-made to achiev The of ro of n ne proteins is beginning to have a clinical imp 8.n1989 .S.Food and Drug Administration(F A)approved system t es tha o 1200 Da mol ight the mos tre FIGURE 2.Release rates of a polymer-magnetic system releasin field min in the absence and in the presenceof an e oyed.Ho whe en placed in a polyme tem for a protein,human growth hor should be available. ncreasing the Rate.The above studies involve using in diseases like diabetes,for example.To examine this we began developing magnetic polymer omposi Ou add wdered drug to it.Without an al magnetic fiel Cutaway ection of delivery microchip(prototyp drug is releas I by slow diffus tic feld is acti ated the compressed.and more drug is released Ever tually.by de th form of a spe ion etching:the reservoirs are filled via inkjet printing or connected to a biosensor.release could be activated on By applying appro ately I V: demand. hed drug proofof To test tthis idea an oscillating g magnetic field was principle release studies have been conducted with single om or mu d h ly on top was attached to the bottom disk The top disk was the n exp A var ety of trig o 30 times higher th those without the magneti erate coul controlled by magnetic field 25. equency gure 2 New Biom In mos t case materials us em with a2-year supply of h rats,an me rot was this enable d progres t ha als bottom disk rotated siving the rats 20-min exposures to the oscilating mag netic field.Blood sugars were e lowered naterials from a engineering.chemical.and biologica ar-norma rol g ndp esigning bette More recently a microchip was designed to deliver We approached this as an engineering design problem asking how onewou de pt one we VOL.33,NO.2,2000/ACCOUNTS OF CHEMICAL RESEARCH 95were very tortuous, slowing the net rate of molecular movement out of the matrix. Using approaches such as controlling polymer molecular weight or composition13 or protein particle size and concentration,14 the pore structures could be predicted and even tailor-made to achieve different release rates. The area of research for slow release of peptides and proteins is beginning to have a clinical impact. In 1989, the U.S. Food and Drug Administration (FDA) approved the first system to slowly release a peptide. These are polymer microspheres that slowly release luteinizing hormone releasing hormone (LHRH) analogues, which are of about 1200 Da molecular weight.15 This is the most widely used system for treating advanced prostate cancer, endometriosis, and precocious puberty. This molecule, if given orally or injected in unencapsulated form, is rapidly destroyed. However, when placed in a polymer matrix, release occurs for 4 months. Soon, a 1-month delivery system for a protein, human growth hormone,16 should be available. Increasing the Rate. The above studies involve using materials to deliver drugs at constant or decreasing release rates. However, increases in release rate might be useful in diseases like diabetes, for example. To examine this, we began developing magnetic polymeric composites. Our thought was to use an elastic material such as ethylenevinyl acetate copolymer as the polymer matrix and add magnetic beads and powdered drug to it. Without an external magnetic field, drug is released by slow diffusion through pores as described above. However, when an oscillating magnetic field is activated, these pores are compressed, and more drug is released.17 Eventually, by designing a triggering system in the form of a special wristwatch-like device that could be programmed or connected to a biosensor, release could be activated on demand. To test this idea, an oscillating magnetic field was designed from two Plexiglas disks placed vertically on top of each other and separated by several inches. A motor was attached to the bottom disk. The top disk was stationary, and the bottom one, which contained magnets, rotated. When exposed to the oscillating magnetic field, the polymer-magnet composites displayed release rates up to 30 times higher than those without the magnetic field. Release rate could be controlled by magnetic field strength and frequency18 (Figure 2). To test this process in vivo, we designed a polymer system with a 2-year supply of insulin and a small magnet. These systems were implanted subcutaneously in diabetic rats, and the same rotating device was used. The rats were placed in small cages on the stationary top disk, while the bottom disk rotated, giving the rats 20-min exposures to the oscillating magnetic field. Blood sugars were lowered to a near-normal level, when the magnetic field was applied. Four control groups exposed showed no such effect.19 More recently, a microchip was designed to deliver drugs20 (Figure 3). The microchip is made of silicon and contains multiple (up to 1000) drug reservoirs, each covered with a thin gold film. The chip is made using photolithography, chemical vapor deposition, and reactive ion etching; the reservoirs are filled via inkjet printing or microinjection. By applying approximately 1 V selectively to any individual reservoir, the gold was dissolved electrochemically, thereby releasing entrapped drug. Proof of principle release studies have been conducted with single or multiple model drugs. This microchip can potentially be regulated by remote control, or eventually a biosensor might be attached to create a smart delivery system. The area of pulsatile drug delivery has attracted the attention of a number of laboratories. A variety of triggering mechanisms including pH, temperature, and specific molecules are under study (for examples, see refs 21- 25). New Biomaterials. In most cases, materials used in medicine were not designed for medical purposes. Usually, these materials were commodity objects utilized by physicians as they attempted to solve medical problems. While this approach has enabled progress, it has also created problems.26 To develop improved materials, we and others have begun asking what is desirable in biomaterials from an engineering, chemical, and biological standpoint, and then synthesizing these materials. One example involves designing better materials for drug delivery. We approached this as an engineering design problem, asking how one would design a polymer to degrade optimally for controlled drug delivery. Ideally, one would FIGURE 2. Release rates of a polymer-magnetic system releasing albumin in the absence and in the presence of an external magnetic field. FIGURE 3. Cutaway section of a drug delivery microchip (prototype device). Biomaterials in Drug Delivery and Tissue Engineering Langer VOL. 33, NO. 2, 2000 / ACCOUNTS OF CHEMICAL RESEARCH 95