正在加载图片...
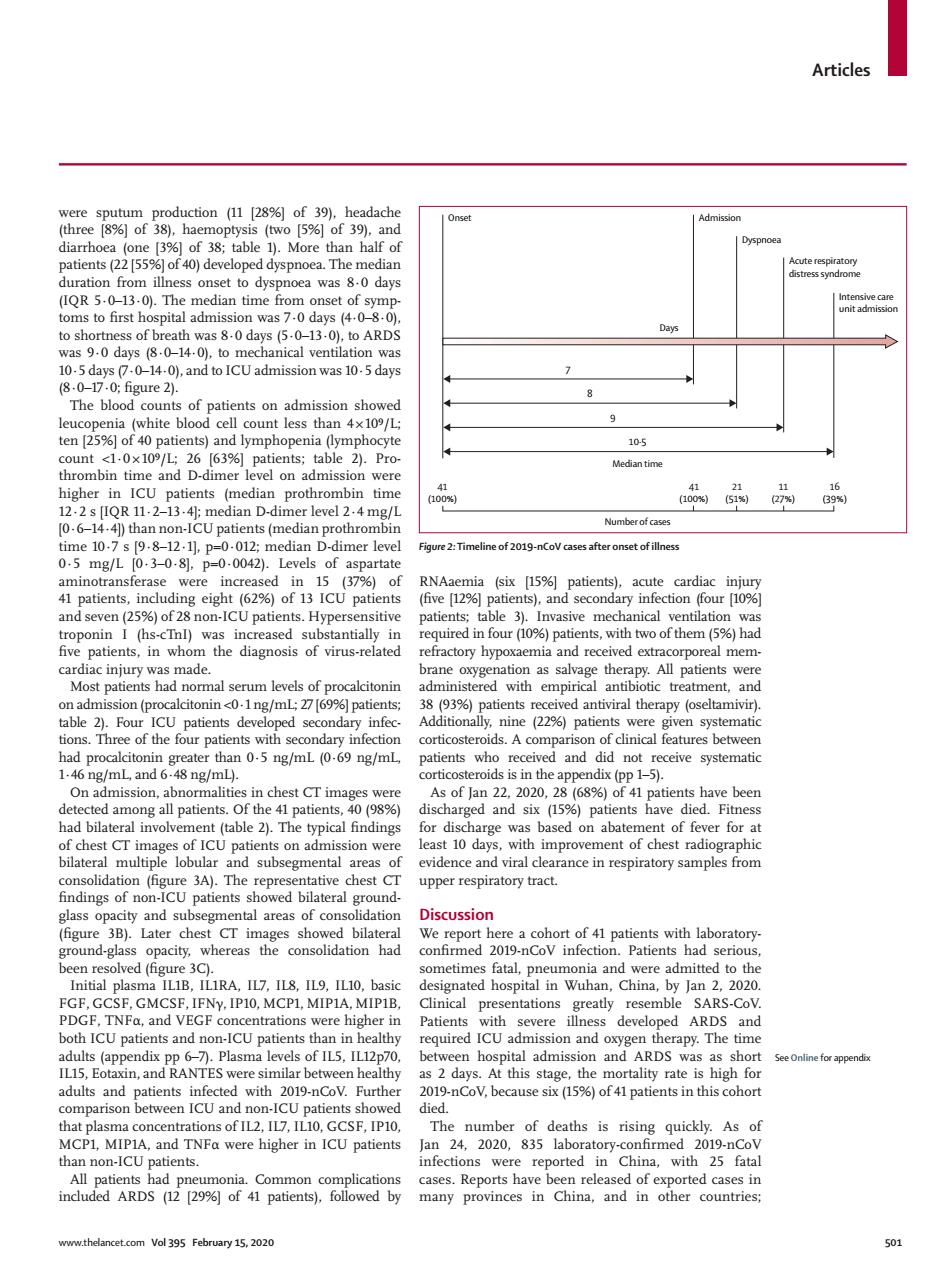
Articles 105 Medin tim 06- iOimetanproth Fure :mei f-Vontof 3037人0-d,838P Uptien Hyp sitive mia and received extrac real mem onin<0-1ng/mL%]pati 5ng/ml(69ng/ml. As of Jan 2.2020.28(6%)of 1 patients have bee all patient 号 for discha d and six (15%)pane ents have e 3A).Th ncdoRae findings of no ents showed bilater (figure Later chest CT im whereas oth ICU patients an CU patients th required ICU admi dobsPpyhe efeppend as2days.At this stage,the mortality rate is high for 9-nCo V,because six (15%)of 41 patients in this cohor ra were 501Articles www.thelancet.com Vol 395 February 15, 2020 501 were sputum production (11 [28%] of 39), headache (three [8%] of 38), haemoptysis (two [5%] of 39), and diarrhoea (one [3%] of 38; table 1). More than half of patients (22 [55%] of 40) developed dyspnoea. The median duration from illness onset to dyspnoea was 8·0 days (IQR 5·0–13·0). The median time from onset of symptoms to first hospital admission was 7·0 days (4·0–8·0), to shortness of breath was 8·0 days (5·0–13·0), to ARDS was 9·0 days (8·0–14·0), to mechanical ventilation was 10·5 days (7·0–14·0), and to ICU admission was 10·5 days (8·0–17·0; figure 2). The blood counts of patients on admission showed leucopenia (white blood cell count less than 4 × 10⁹/L; ten [25%] of 40 patients) and lymphopenia (lymphocyte count <1·0 × 10⁹/L; 26 [63%] patients; table 2). Prothrombin time and D-dimer level on admission were higher in ICU patients (median prothrombin time 12·2 s [IQR 11·2–13·4]; median D-dimer level 2·4 mg/L [0·6–14·4]) than non-ICU patients (median prothrombin time 10·7 s [9·8–12·1], p=0·012; median D-dimer level 0·5 mg/L [0·3–0·8], p=0·0042). Levels of aspartate aminotransferase were increased in 15 (37%) of 41 patients, including eight (62%) of 13 ICU patients and seven (25%) of 28 non-ICU patients. Hypersensitive troponin I (hs-cTnI) was increased substantially in five patients, in whom the diagnosis of virus-related cardiac injury was made. Most patients had normal serum levels of procalcitonin on admission (procalcitonin <0·1 ng/mL; 27 [69%] patients; table 2). Four ICU patients developed secondary infections. Three of the four patients with secondary infection had procalcitonin greater than 0·5 ng/mL (0·69 ng/mL, 1·46 ng/mL, and 6·48 ng/mL). On admission, abnormalities in chest CT images were detected among all patients. Of the 41 patients, 40 (98%) had bilateral involvement (table 2). The typical findings of chest CT images of ICU patients on admission were bilateral multiple lobular and subsegmental areas of consolidation (figure 3A). The representative chest CT findings of non-ICU patients showed bilateral groundglass opacity and subsegmental areas of consolidation (figure 3B). Later chest CT images showed bilateral ground-glass opacity, whereas the consolidation had been resolved (figure 3C). Initial plasma IL1B, IL1RA, IL7, IL8, IL9, IL10, basic FGF, GCSF, GMCSF, IFNγ, IP10, MCP1, MIP1A, MIP1B, PDGF, TNFα, and VEGF concentrations were higher in both ICU patients and non-ICU patients than in healthy adults (appendix pp 6–7). Plasma levels of IL5, IL12p70, IL15, Eotaxin, and RANTES were similar between healthy adults and patients infected with 2019-nCoV. Further comparison between ICU and non-ICU patients showed that plasma concentrations of IL2, IL7, IL10, GCSF, IP10, MCP1, MIP1A, and TNFα were higher in ICU patients than non-ICU patients. All patients had pneumonia. Common complications included ARDS (12 [29%] of 41 patients), followed by RNAaemia (six [15%] patients), acute cardiac injury (five [12%] patients), and secondary infection (four [10%] patients; table 3). Invasive mechanical ventilation was required in four (10%) patients, with two of them (5%) had refractory hypoxaemia and received extracorporeal membrane oxygenation as salvage therapy. All patients were administered with empirical antibiotic treatment, and 38 (93%) patients received antiviral therapy (oseltamivir). Additionally, nine (22%) patients were given systematic corticosteroids. A comparison of clinical features between patients who received and did not receive systematic corticosteroids is in the appendix (pp 1–5). As of Jan 22, 2020, 28 (68%) of 41 patients have been discharged and six (15%) patients have died. Fitness for discharge was based on abatement of fever for at least 10 days, with improvement of chest radiographic evidence and viral clearance in respiratory samples from upper respiratory tract. Discussion We report here a cohort of 41 patients with laboratoryconfirmed 2019-nCoV infection. Patients had serious, sometimes fatal, pneumonia and were admitted to the designated hospital in Wuhan, China, by Jan 2, 2020. Clinical presentations greatly resemble SARS-CoV. Patients with severe illness developed ARDS and required ICU admission and oxygen therapy. The time between hospital admission and ARDS was as short as 2 days. At this stage, the mortality rate is high for 2019-nCoV, because six (15%) of 41 patients in this cohort died. The number of deaths is rising quickly. As of Jan 24, 2020, 835 laboratory-confirmed 2019-nCoV infections were reported in China, with 25 fatal cases. Reports have been released of exported cases in many provinces in China, and in other countries; Figure 2: Timeline of 2019-nCoV cases after onset of illness Onset Admission Dyspnoea Acute respiratory distress syndrome Intensive care unit admission 7 8 9 10·5 Median time Number of cases Days 41 (100%) 41 (100%) 21 (51%) 11 (27%) 16 (39%) See Online for appendix