正在加载图片...
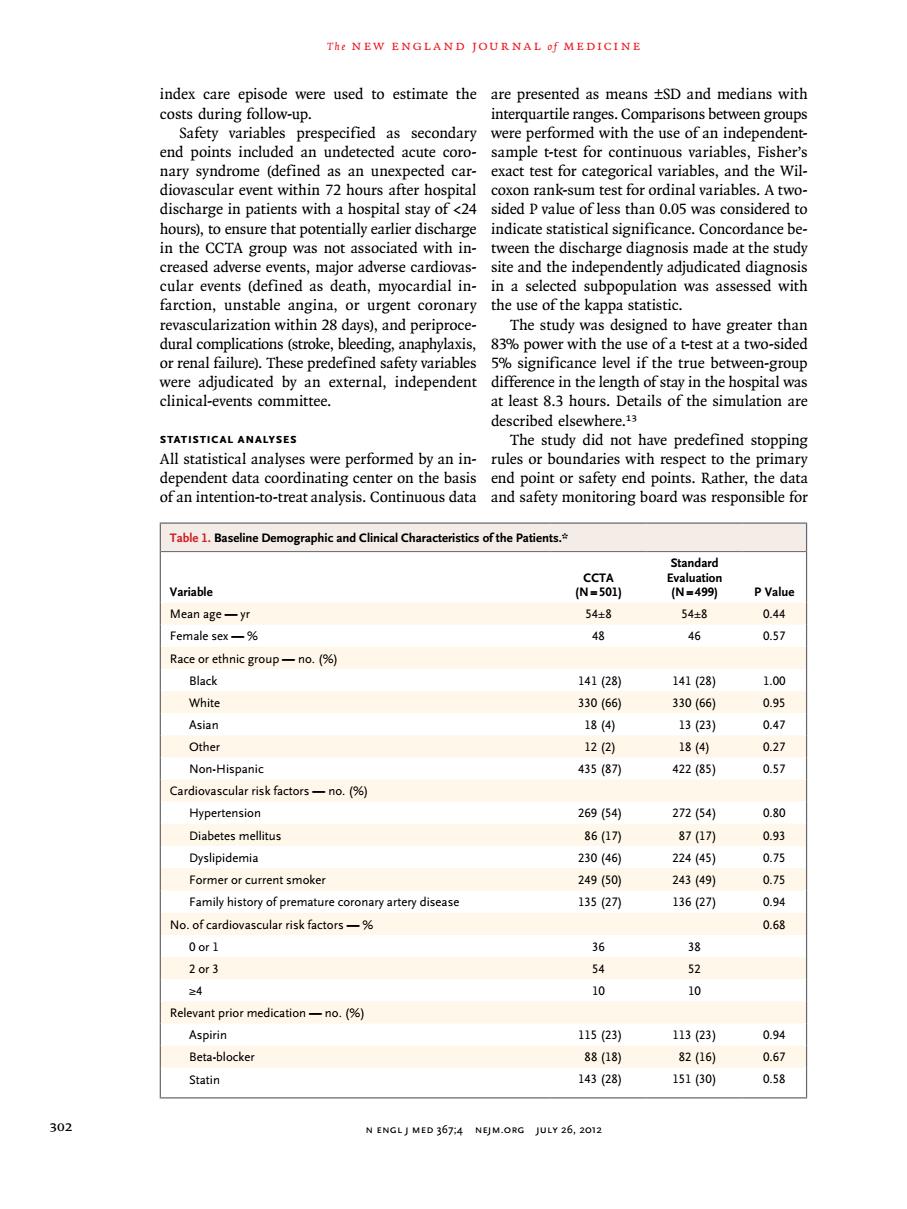
The NEW ENGLAND JOURNAL f MEDICINE index care episode were used to estimate the are presented as means tSD and medians with costs during follow-up. interquartile ranges.Comparisons between groups Safety variables prespecified as secondary were performed with the use of an in end points inc undetecte acute cor sample est for con nuou unex discharee in patients with a hos nital stay of 24 sided pvalue of less than 005 wa hours)to ensure that potentially earlier discharge indicate statistical significance concordance be in the CCTA group was not associated with in-tween the discharge diagnosis made at the study creased adverse events,major adverse cardiovas- site and the independently adjudicated diagnosi ined as death,myocardial in- n a select subpopula was assessed with urgent coronary the app o ha ter or renal failure).These variables mnificance level if the true betw were adjudicated by an external,independent difference in the length of stay in the hospital was clinical-events committee. at least 8.3 hours.Details of the simulation are described elsewhere. E The study did not ave predefined yses we e performed by yanin rules or b ect t o-t-Connouat Table 1.Baseline Demographic and Clinical Chara ristics of the Patients.* Standard Variable 499 Mean age-yr 54± 54 Female sex-% 8 46 0.57 Race or ethnic group-no.(96) Black 14128 141(28) 1.00 White 330166 330(66) 只 Asian 323 Non-Hispanic 435(87 422(85) Cardiovascular risk factors-no.(% Hypertension 26954 27254) Diabetes mellitus 8617刀 870刀 093 Dyslipidemia 230(46 2445 0.75 2439 Family history of premature coronary artery disease 13627 0 No.of cardiovascular risk factors- 0.63 Oor1 38 2or3 52 y 0 10 Relevant prior medication-. Aspirin 152 Beta-blocker 88(18) 82(16) Statin 143(28) 151(30) 0.58 N ENGLJ MED 367:4 NEJM.ORG JULY 26,2012 T h e n e w e ngl a nd j o u r na l o f m e dic i n e 302 n engl j med 367;4 nejm.org july 26, 2012 index care episode were used to estimate the costs during follow-up. Safety variables prespecified as secondary end points included an undetected acute coronary syndrome (defined as an unexpected cardiovascular event within 72 hours after hospital discharge in patients with a hospital stay of <24 hours), to ensure that potentially earlier discharge in the CCTA group was not associated with increased adverse events, major adverse cardiovascular events (defined as death, myocardial infarction, unstable angina, or urgent coronary revascularization within 28 days), and periprocedural complications (stroke, bleeding, anaphylaxis, or renal failure). These predefined safety variables were adjudicated by an external, independent clinical-events committee. Statistical Analyses All statistical analyses were performed by an independent data coordinating center on the basis of an intention-to-treat analysis. Continuous data are presented as means ±SD and medians with interquartile ranges. Comparisons between groups were performed with the use of an independentsample t-test for continuous variables, Fisher’s exact test for categorical variables, and the Wilcoxon rank-sum test for ordinal variables. A twosided P value of less than 0.05 was considered to indicate statistical significance. Concordance between the discharge diagnosis made at the study site and the independently adjudicated diagnosis in a selected subpopulation was assessed with the use of the kappa statistic. The study was designed to have greater than 83% power with the use of a t-test at a two-sided 5% significance level if the true between-group difference in the length of stay in the hospital was at least 8.3 hours. Details of the simulation are described elsewhere.13 The study did not have predefined stopping rules or boundaries with respect to the primary end point or safety end points. Rather, the data and safety monitoring board was responsible for Table 1. Baseline Demographic and Clinical Characteristics of the Patients.* Variable CCTA (N=501) Standard Evaluation (N=499) P Value Mean age — yr 54±8 54±8 0.44 Female sex — % 48 46 0.57 Race or ethnic group — no. (%) Black 141 (28) 141 (28) 1.00 White 330 (66) 330 (66) 0.95 Asian 18 (4) 13 (23) 0.47 Other 12 (2) 18 (4) 0.27 Non-Hispanic 435 (87) 422 (85) 0.57 Cardiovascular risk factors — no. (%) Hypertension 269 (54) 272 (54) 0.80 Diabetes mellitus 86 (17) 87 (17) 0.93 Dyslipidemia 230 (46) 224 (45) 0.75 Former or current smoker 249 (50) 243 (49) 0.75 Family history of premature coronary artery disease 135 (27) 136 (27) 0.94 No. of cardiovascular risk factors — % 0.68 0 or 1 36 38 2 or 3 54 52 ≥4 10 10 Relevant prior medication — no. (%) Aspirin 115 (23) 113 (23) 0.94 Beta-blocker 88 (18) 82 (16) 0.67 Statin 143 (28) 151 (30) 0.58