The Use of High-Energy Protons in Cancer Therapy 王鹏程印
The Use of High-Energy Protons in Cancer Therapy
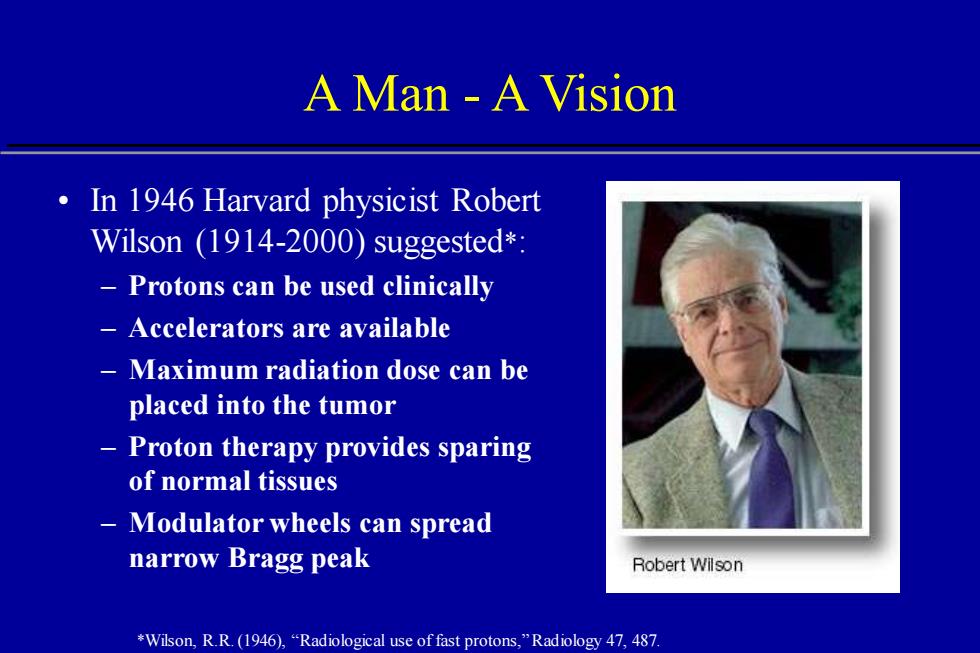
A Man A Vision In 1946 Harvard physicist Robert Wilson (1914-2000)suggested*: Protons can be used clinically Accelerators are available Maximum radiation dose can be placed into the tumor Proton therapy provides sparing of normal tissues Modulator wheels can spread narrow Bragg peak Robert Wilson *Wilson,R.R.(1946),"Radiological use of fast protons,"Radiology 47,487
A Man - A Vision • In 1946 Harvard physicist Robert Wilson (1914-2000) suggested*: – Protons can be used clinically – Accelerators are available – Maximum radiation dose can be placed into the tumor – Proton therapy provides sparing of normal tissues – Modulator wheels can spread narrow Bragg peak *Wilson, R.R. (1946), “Radiological use of fast protons,” Radiology 47, 487
History of Proton Beam Therapy 1946 R.Wilson suggests use of protons 1954 First treatment of pituitary tumors 1958 First use of protons as a neurosurgical tool 1967 First large-field proton treatments in Sweden 1974 Large-field fractionated proton treatments program begins at HCL,Cambridge,MA 1990 First hospital-based proton treatment center opens at Loma Linda University Medical Center
History of Proton Beam Therapy • 1946 R. Wilson suggests use of protons • 1954 First treatment of pituitary tumors • 1958 First use of protons as a neurosurgical tool • 1967 First large-field proton treatments in Sweden • 1974 Large-field fractionated proton treatments program begins at HCL, Cambridge, MA • 1990 First hospital-based proton treatment center opens at Loma Linda University Medical Center

World Wide Proton Treatments* Dubna(1967) 172 CANADA GER POL Moscow (1969) 3414 St.Petersburg (1969)1029 NORTH UNITED STATES Uppsala(1957): 309 CHINA HCL(1961) PSI(1984) 3935 LLUMC (1990) 6174 Clatterbridge(1989):1033 Chiba (1979) 133 INDIA 6174 Nice(1991): 1590 Tsukuba (1983) 700 Orsay (1991): 1894 Kashiwa (1998) 75 Berlin(1998) 166 A N。6 BRAZIL AUSTRALIA NAC(1993) 0/72H SOUTH PACIFIC ATLANTIE 398 *from:Particles,Newsletter (Ed J.Sisterson),No.28.July 2001
World Wide Proton Treatments* LLUMC (1990) 6174 HCL (1961) 6174 Uppsala (1957): 309 PSI (1984): 3935 Clatterbridge(1989): 1033 Nice (1991): 1590 Orsay (1991): 1894 Berlin (1998): 166 Chiba (1979) 133 Tsukuba (1983) 700 Kashiwa (1998) 75 NAC (1993) 398 Dubna (1967) 172 Moscow (1969) 3414 St. Petersburg (1969) 1029 *from: Particles, Newsletter (Ed J. Sisterson), No. 28. July 2001
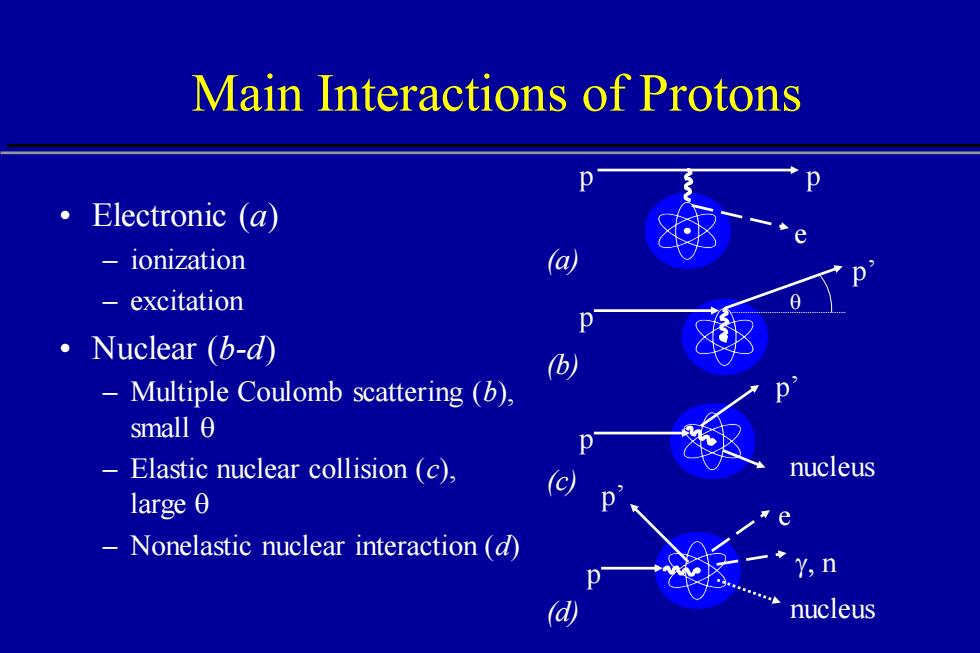
Main Interactions of Protons ·Electronic(a) ionization 一 excitation ·Nuclear(b-d Multiple Coulomb scattering (b). small 0 Elastic nuclear collision (c), nucleus large 0 Nonelastic nuclear interaction (d) Y,n d nucleus
Main Interactions of Protons • Electronic (a) – ionization – excitation • Nuclear (b-d) – Multiple Coulomb scattering (b), small q – Elastic nuclear collision (c), large q – Nonelastic nuclear interaction (d) e p p p’ p p p’ nucleus g, n p’ p e nucleus (b) (c) (d) (a) q
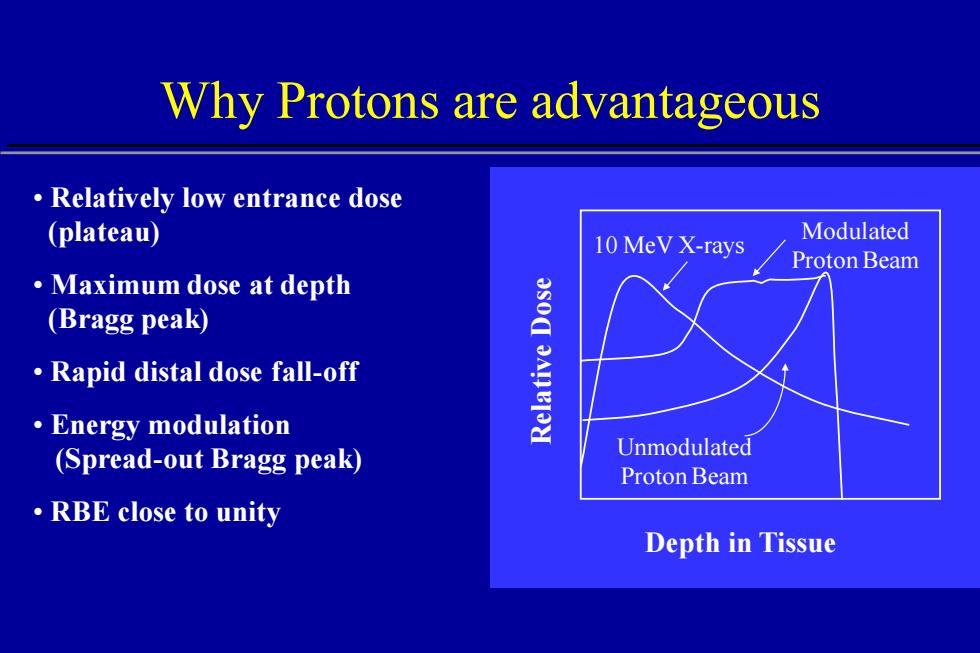
Why Protons are advantageous Relatively low entrance dose (plateau) 10 MeV X-rays Modulated Proton Beam ·Maximum dose at depth (Bragg peak) Rapid distal dose fall-off ·Energy modulation (Spread-out Bragg peak) Unmodulated Proton Beam ·RBE close to unity Depth in Tissue
Why Protons are advantageous • Relatively low entrance dose (plateau) • Maximum dose at depth (Bragg peak) • Rapid distal dose fall-off • Energy modulation (Spread-out Bragg peak) • RBE close to unity Depth in Tissue Relative Dose 10 MeV X-rays Modulated Proton Beam Unmodulated Proton Beam
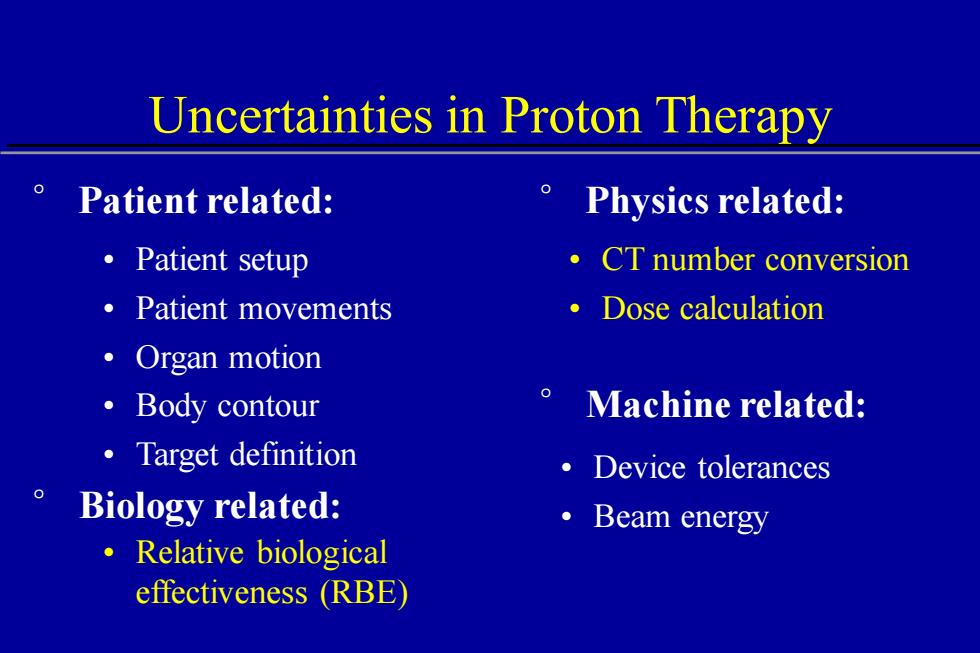
Uncertainties in Proton Therapy Patient related: Physics related: ·Patient setup ·CT number conversion ·Patient movements ·Dose calculation 。Organ motion ·Body contour Machine related: 。Target definition ·Device tolerances Biology related: ·Beam energy ·Relative biological effectiveness (RBE)
Uncertainties in Proton Therapy • Patient setup • Patient movements • Organ motion • Body contour • Target definition • Relative biological effectiveness (RBE) • Device tolerances ° Biology related: • Beam energy ° Patient related: ° Physics related: • CT number conversion • Dose calculation ° Machine related:
Treatment Planning Acquisition of imaging data(CT,MRI) Conversion of CT values into stopping power Delineation of regions of interest Selection of proton beam directions :cdmNe>
Treatment Planning • Acquisition of imaging data (CT, MRI) • Conversion of CT values into stopping power • Delineation of regions of interest • Selection of proton beam directions • Design of each beam • Optimization of the plan
Treatment Delivery Fabrication of apertures and boluses ·Beam calibration Alignment of patient using DRRs Computer-controlled dose delivery
Treatment Delivery • Fabrication of apertures and boluses • Beam calibration • Alignment of patient using DRRs • Computer-controlled dose delivery
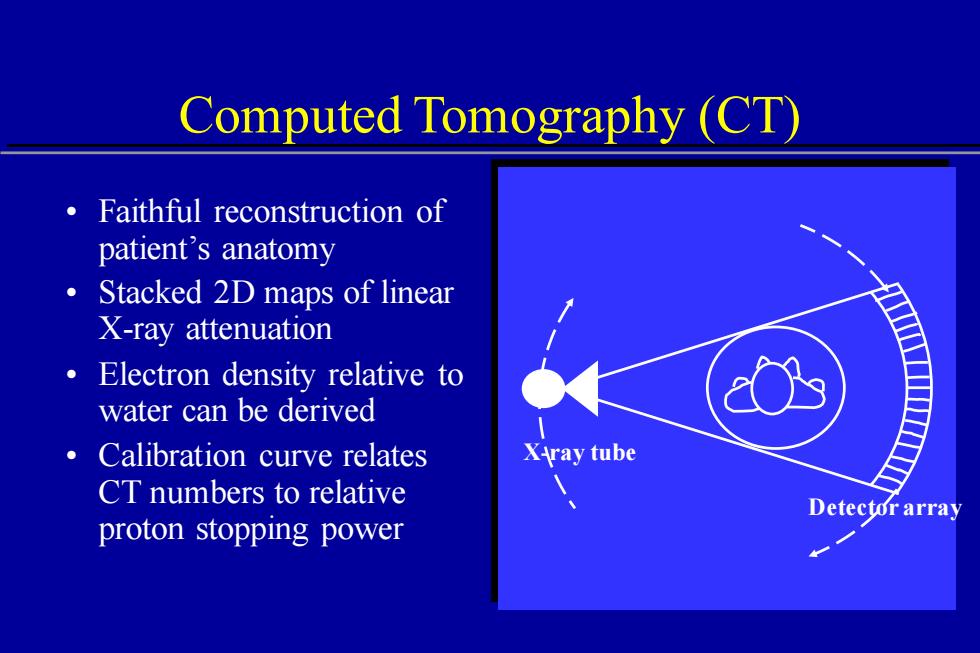
Computed Tomography (CT) Faithful reconstruction of patient's anatomy Stacked 2D maps of linear X-ray attenuation Electron density relative to water can be derived Calibration curve relates XAray tube CT numbers to relative Detector array proton stopping power
Computed Tomography (CT) X-ray tube Detector array • Faithful reconstruction of patient’s anatomy • Stacked 2D maps of linear X-ray attenuation • Electron density relative to water can be derived • Calibration curve relates CT numbers to relative proton stopping power