Antidepressant Agents William Z.Potter,MD,PhD,Leo E.Hollister,MD* Introduction Major depression is one of the most common psychiatric disorders.At any given moment,about 3-5%of the population is depressed(point prevalence),and an estimated 10%of people may become depressed during their lives(lifetime prevalence).The symptoms of depression are often subtle and unrecognized both by patients and by physicians.Patients with vague complaints that resist explanation as manifestations of somatic disorders and those who might be simplistically described as "neurotic"should be suspected of being depressed. Depression is a heterogeneous disorder that has been characterized and classified in a variety of ways.According to the American Psychiatric Association's modified fourth edition (2000)of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR),several diagnoses of affective disorders are possible.Major depression and dysthymia(minor)are pure depressive syndromes,whereas bipolar disorder and cyclothymic disorder signify depression in association with mania.A simplified classification based on presumed origin is as follows:(1)brief reactive or secondary depression(most common),occurring in response to real stimuli such as grief,illness, etc;(2)melancholic and recurrent depression,a genetically determined biochemical disorder manifested by an inability to experience ordinary pleasure or to cope with ordinary life events;and (3)depression associated with bipolar affective (manic-depressive)disorder.Because safe antidepressants are now available,almost any individual with several symptoms of depression that persist beyond a few weeks is a candidate for pharmacologic treatment.Intensive efforts to formalize guidelines for the treatment of depression have been pursued for more than a decade,resulting in guidelines from the American Psychiatric Association,the Agency for Health Care Policy and Research,and the World Federation of Societies of Biological Psychiatry. Pharmacologic treatment is emphasized,although a continuing role for electroconvulsive therapy for delusional or severe forms of life-threatening depression is also noted. *Deceased. The Pathogenesis of Major Depression:The Amine Hypothesis and Subsequent Developments Soon after the introduction of reserpine in the early 1950s,it became apparent that the drug could induce depression.Studies revealed that the principal mechanism of action of reserpine was to inhibit the neuronal storage of amine neurotransmitters such as serotonin and norepinephrine.Reserpine induced depression and depleted stores of amine neurotransmitters;therefore,it was reasoned,depression must be associated with decreased functional amine-dependent synaptic transmission.This idea provided
Antidepressant Agents ¾ William Z. Potter, MD, PhD, & Leo E. Hollister, MD* Introduction Major depression is one of the most common psychiatric disorders. At any given moment, about 3-5% of the population is depressed (point prevalence), and an estimated 10% of people may become depressed during their lives (lifetime prevalence). The symptoms of depression are often subtle and unrecognized both by patients and by physicians. Patients with vague complaints that resist explanation as manifestations of somatic disorders and those who might be simplistically described as "neurotic" should be suspected of being depressed. Depression is a heterogeneous disorder that has been characterized and classified in a variety of ways. According to the American Psychiatric Association's modified fourth edition (2000) of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR), several diagnoses of affective disorders are possible. Major depression and dysthymia (minor) are pure depressive syndromes, whereas bipolar disorder and cyclothymic disorder signify depression in association with mania. A simplified classification based on presumed origin is as follows: (1) brief reactive or secondary depression (most common), occurring in response to real stimuli such as grief, illness, etc; (2) melancholic and recurrent depression, a genetically determined biochemical disorder manifested by an inability to experience ordinary pleasure or to cope with ordinary life events; and (3) depression associated with bipolar affective (manic-depressive) disorder. Because safe antidepressants are now available, almost any individual with several symptoms of depression that persist beyond a few weeks is a candidate for pharmacologic treatment. Intensive efforts to formalize guidelines for the treatment of depression have been pursued for more than a decade, resulting in guidelines from the American Psychiatric Association, the Agency for Health Care Policy and Research, and the World Federation of Societies of Biological Psychiatry. Pharmacologic treatment is emphasized, although a continuing role for electroconvulsive therapy for delusional or severe forms of life-threatening depression is also noted. *Deceased. The Pathogenesis of Major Depression: The Amine Hypothesis and Subsequent Developments Soon after the introduction of reserpine in the early 1950s, it became apparent that the drug could induce depression. Studies revealed that the principal mechanism of action of reserpine was to inhibit the neuronal storage of amine neurotransmitters such as serotonin and norepinephrine. Reserpine induced depression and depleted stores of amine neurotransmitters; therefore, it was reasoned, depression must be associated with decreased functional amine-dependent synaptic transmission. This idea provided
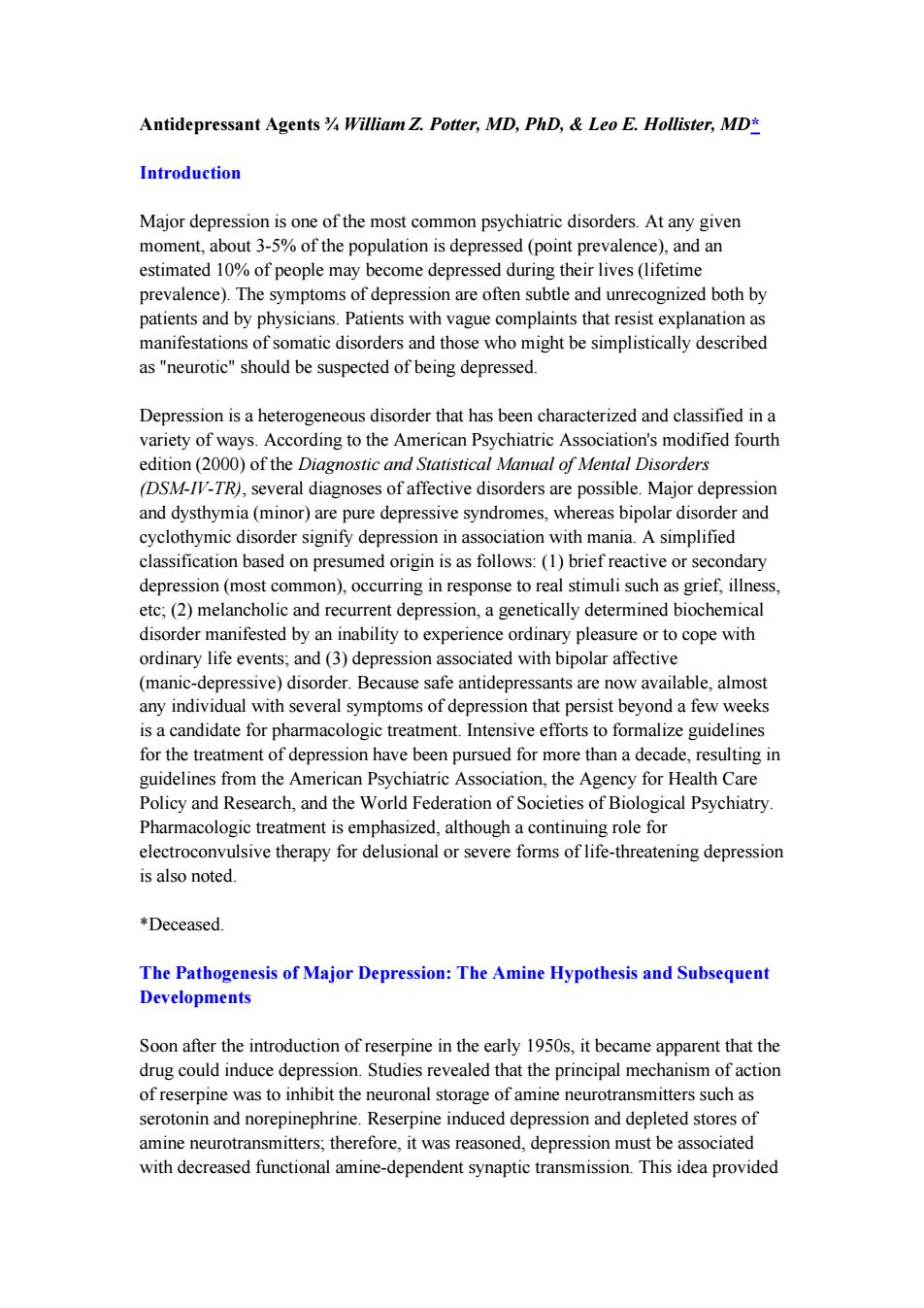
the basis for what became known as the amine hypothesis of depression.By extension, drugs that increased amine function in appropriate synaptic areas would relieve depression.A major puzzle in applying this hypothesis was the fact that although the pharmacologic actions of both tricyclic and monoamine oxidase(MAO)inhibitor classes of antidepressants are prompt,the clinical effects require weeks to become manifest.Attempts have been made to explain this observation by invoking slow compensatory responses to the initial blockade of amine reuptake or MAO inhibition (see below). Current brain imaging and biochemical studies in patients do not support a single biologic abnormality as common to most depressions.Rather,prevailing hypotheses emphasize an underlying role for several brain circuits that have a propensity to become dysfunctional,especially following certain stressors,in individuals with a range of genetic predispositions.It is likely that several pathophysiologic processes will ultimately be identified to account for the presentation of what is now termed major depression. Nevertheless,the amine hypothesis has provided the major experimental models for the discovery of new antidepressant drugs.As a result,all currently available antidepressants,except bupropion,are classified as having their primary actions on the metabolism,reuptake,or selective receptor antagonism of serotonin, norepinephrine,or both. I.BASIC PHARMACOLOGY OF ANTIDEPRESSANTS Chemistry A variety of chemical structures have been found to have antidepressant activity.With the exception of bupropion,however,the core antidepressant action of even the newest agents derives from mechanisms proposed for antidepressants that were introduced four decades ago. A.TRICYCLIC ANTIDEPRESSANTS (TCAS) Tricyclic antidepressants%so called because of the characteristic three-ring nucleus (Figure 30-1)have been used clinically for four decades.They closely resemble the phenothiazines chemically and,to a lesser extent,pharmacologically.Like the phenothiazines,tricyclics were first thought to be useful as antihistamines with sedative properties.The discovery of their antidepressant properties was a fortuitous clinical observation.Imipramine and amitriptyline are the prototypical drugs of the class as mixed norepinephrine and serotonin uptake inhibitors,although they also have several other effects. B.SECOND-GENERATION AND SUBSEQUENT AGENTS
the basis for what became known as the amine hypothesis of depression. By extension, drugs that increased amine function in appropriate synaptic areas would relieve depression. A major puzzle in applying this hypothesis was the fact that although the pharmacologic actions of both tricyclic and monoamine oxidase (MAO) inhibitor classes of antidepressants are prompt, the clinical effects require weeks to become manifest. Attempts have been made to explain this observation by invoking slow compensatory responses to the initial blockade of amine reuptake or MAO inhibition (see below). Current brain imaging and biochemical studies in patients do not support a single biologic abnormality as common to most depressions. Rather, prevailing hypotheses emphasize an underlying role for several brain circuits that have a propensity to become dysfunctional, especially following certain stressors, in individuals with a range of genetic predispositions. It is likely that several pathophysiologic processes will ultimately be identified to account for the presentation of what is now termed major depression. Nevertheless, the amine hypothesis has provided the major experimental models for the discovery of new antidepressant drugs. As a result, all currently available antidepressants, except bupropion, are classified as having their primary actions on the metabolism, reuptake, or selective receptor antagonism of serotonin, norepinephrine, or both. I. BASIC PHARMACOLOGY OF ANTIDEPRESSANTS Chemistry A variety of chemical structures have been found to have antidepressant activity. With the exception of bupropion, however, the core antidepressant action of even the newest agents derives from mechanisms proposed for antidepressants that were introduced four decades ago. A. TRICYCLIC ANTIDEPRESSANTS (TCAS) Tricyclic antidepressants¾so called because of the characteristic three-ring nucleus (Figure 30-1) have been used clinically for four decades. They closely resemble the phenothiazines chemically and, to a lesser extent, pharmacologically. Like the phenothiazines, tricyclics were first thought to be useful as antihistamines with sedative properties. The discovery of their antidepressant properties was a fortuitous clinical observation. Imipramine and amitriptyline are the prototypical drugs of the class as mixed norepinephrine and serotonin uptake inhibitors, although they also have several other effects. B. SECOND-GENERATION AND SUBSEQUENT AGENTS
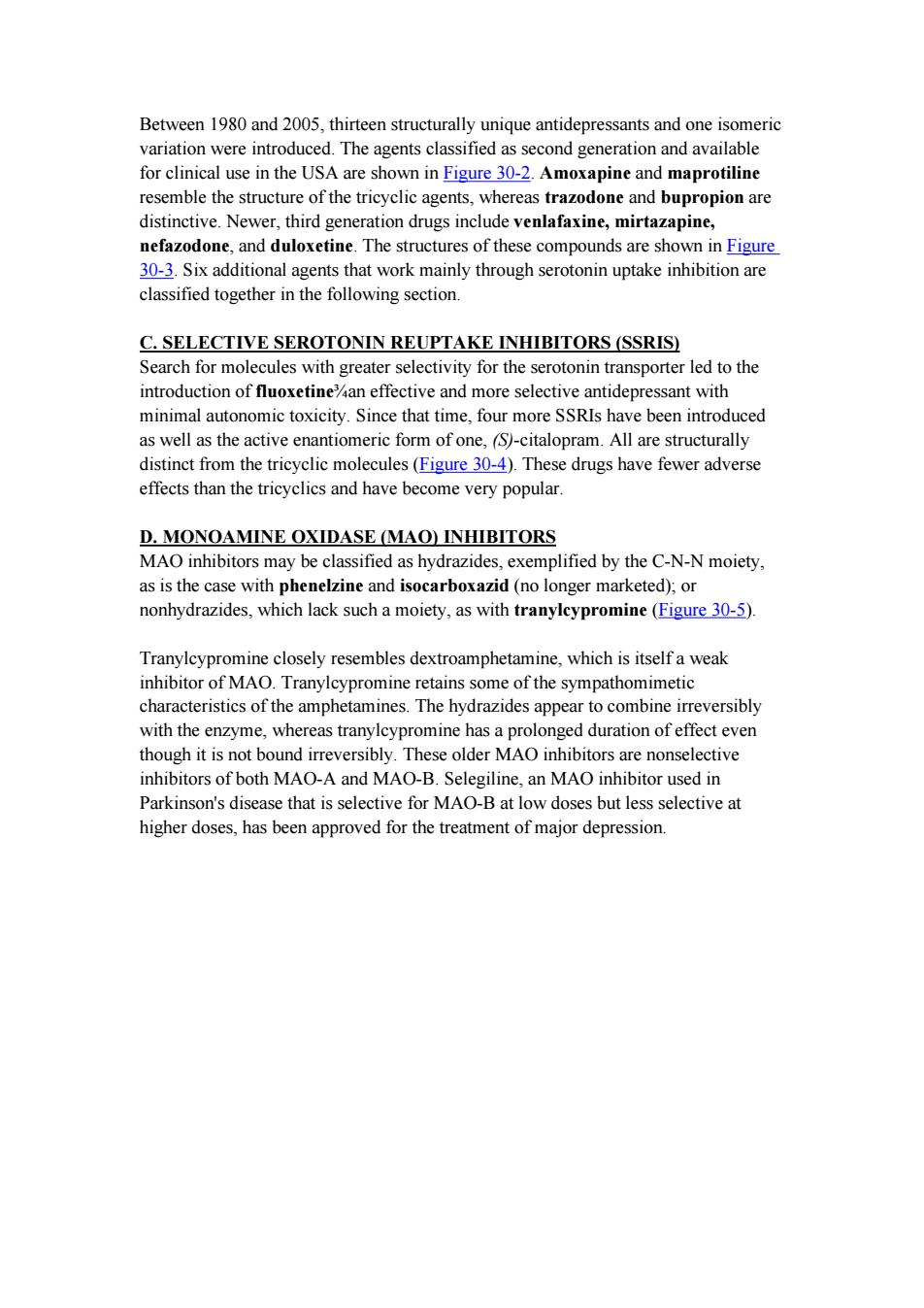
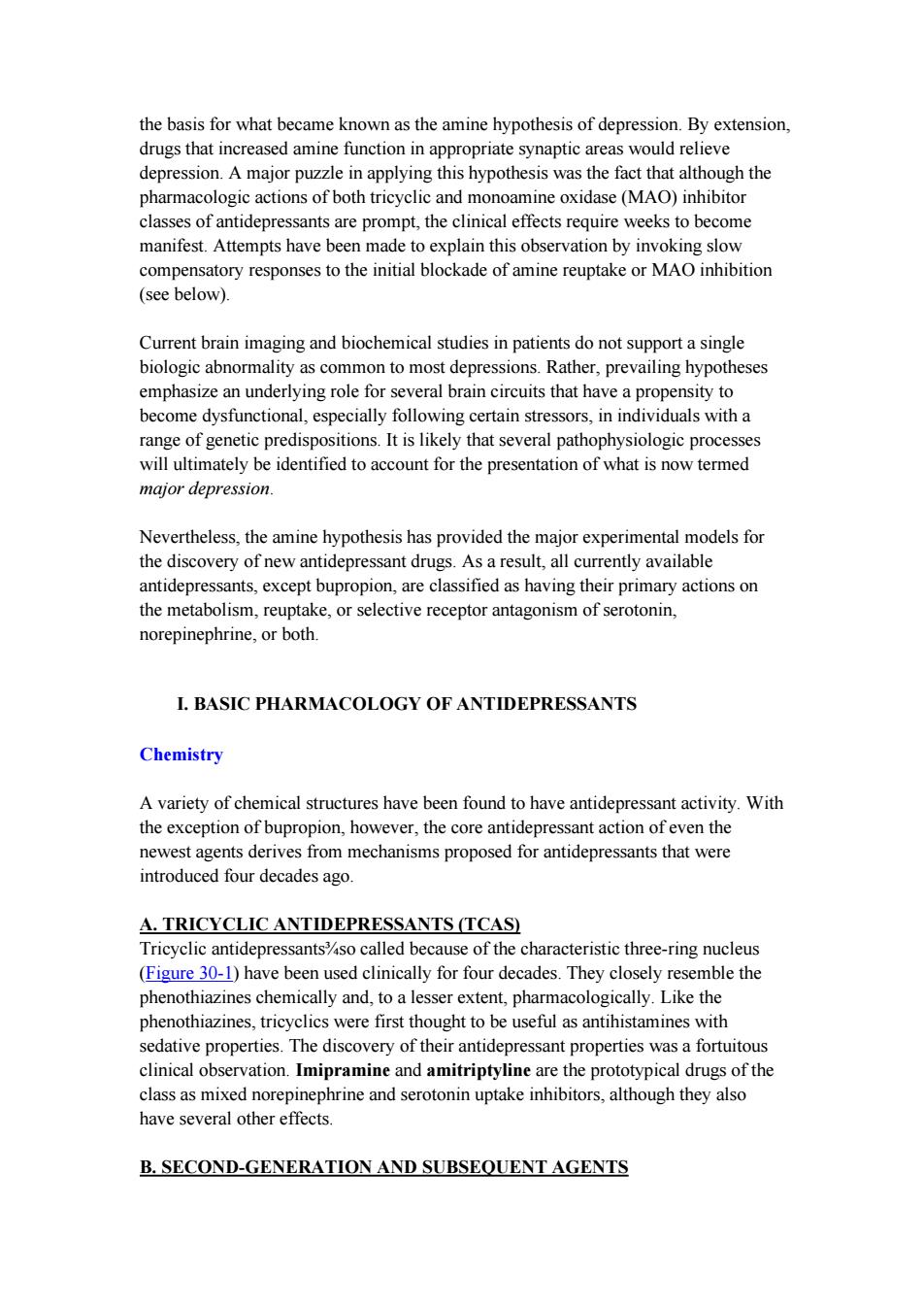
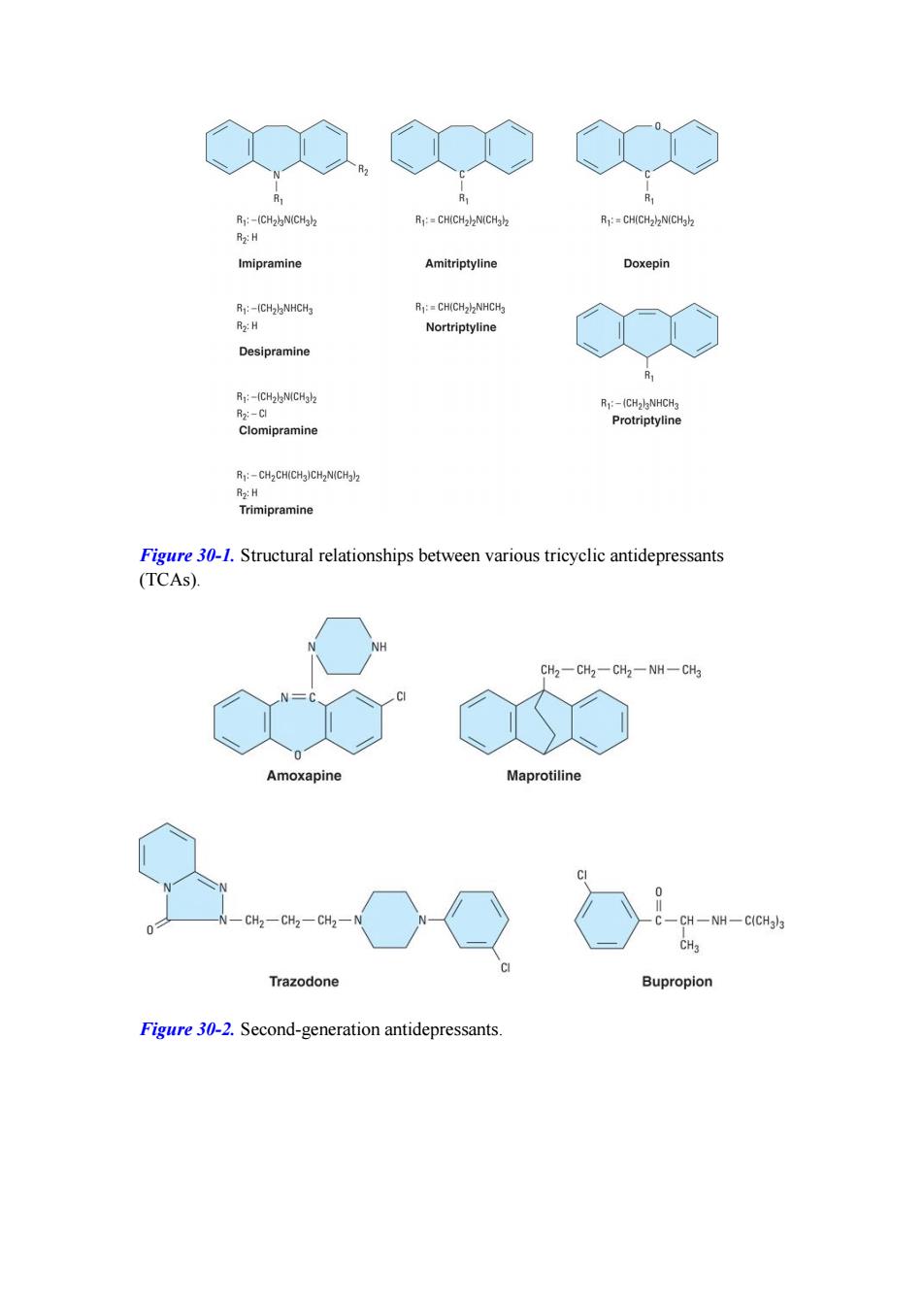
Between 1980 and 2005,thirteen structurally unique antidepressants and one isomeric variation were introduced.The agents classified as second generation and available for clinical use in the USA are shown in Figure 30-2.Amoxapine and maprotiline resemble the structure of the tricyclic agents,whereas trazodone and bupropion are distinctive.Newer,third generation drugs include venlafaxine,mirtazapine, nefazodone,and duloxetine.The structures of these compounds are shown in Figure 30-3.Six additional agents that work mainly through serotonin uptake inhibition are classified together in the following section. C.SELECTIVE SEROTONIN REUPTAKE INHIBITORS (SSRIS) Search for molecules with greater selectivity for the serotonin transporter led to the introduction of fluoxetine%an effective and more selective antidepressant with minimal autonomic toxicity.Since that time,four more SSRIs have been introduced as well as the active enantiomeric form of one,(S)-citalopram.All are structurally distinct from the tricyclic molecules(Figure 30-4).These drugs have fewer adverse effects than the tricyclics and have become very popular. D.MONOAMINE OXIDASE (MAO)INHIBITORS MAO inhibitors may be classified as hydrazides,exemplified by the C-N-N moiety, as is the case with phenelzine and isocarboxazid(no longer marketed);or nonhydrazides,which lack such a moiety,as with tranylcypromine(Figure 30-5). Tranylcypromine closely resembles dextroamphetamine,which is itself a weak inhibitor of MAO.Tranylcypromine retains some of the sympathomimetic characteristics of the amphetamines.The hydrazides appear to combine irreversibly with the enzyme,whereas tranylcypromine has a prolonged duration of effect even though it is not bound irreversibly.These older MAO inhibitors are nonselective inhibitors of both MAO-A and MAO-B.Selegiline,an MAO inhibitor used in Parkinson's disease that is selective for MAO-B at low doses but less selective at higher doses,has been approved for the treatment of major depression
Between 1980 and 2005, thirteen structurally unique antidepressants and one isomeric variation were introduced. The agents classified as second generation and available for clinical use in the USA are shown in Figure 30-2. Amoxapine and maprotiline resemble the structure of the tricyclic agents, whereas trazodone and bupropion are distinctive. Newer, third generation drugs include venlafaxine, mirtazapine, nefazodone, and duloxetine. The structures of these compounds are shown in Figure 30-3. Six additional agents that work mainly through serotonin uptake inhibition are classified together in the following section. C. SELECTIVE SEROTONIN REUPTAKE INHIBITORS (SSRIS) Search for molecules with greater selectivity for the serotonin transporter led to the introduction of fluoxetine¾an effective and more selective antidepressant with minimal autonomic toxicity. Since that time, four more SSRIs have been introduced as well as the active enantiomeric form of one, (S)-citalopram. All are structurally distinct from the tricyclic molecules (Figure 30-4). These drugs have fewer adverse effects than the tricyclics and have become very popular. D. MONOAMINE OXIDASE (MAO) INHIBITORS MAO inhibitors may be classified as hydrazides, exemplified by the C-N-N moiety, as is the case with phenelzine and isocarboxazid (no longer marketed); or nonhydrazides, which lack such a moiety, as with tranylcypromine (Figure 30-5). Tranylcypromine closely resembles dextroamphetamine, which is itself a weak inhibitor of MAO. Tranylcypromine retains some of the sympathomimetic characteristics of the amphetamines. The hydrazides appear to combine irreversibly with the enzyme, whereas tranylcypromine has a prolonged duration of effect even though it is not bound irreversibly. These older MAO inhibitors are nonselective inhibitors of both MAO-A and MAO-B. Selegiline, an MAO inhibitor used in Parkinson's disease that is selective for MAO-B at low doses but less selective at higher doses, has been approved for the treatment of major depression
R:-(CH2)N(CH3)2 R:=CH(CH2)2N(CH3h2 R1:=CH(CH2)N(CHab R2:H Imipramine Amitriptyline Doxepin Rj:-(CH2lNHCH3 R:=CH(CH22NHCH3 R2:H Nortriptyline Desipramine R:-(CH2lN(CHgl2 R:-(CH2lgNHCH3 R2:-C Protriptyline Clomipramine R:-CH2CH(CH3)CH2N(CH3)2 R2:H Trimipramine Figure 30-1.Structural relationships between various tricyclic antidepressants (TCAs). NH CH2一CH2一CH2一NH一CH3 Amoxapine Maprotiline 0 CH2-CH2一CH2一 CH -NH一C(CH3)3 CHa Trazodone Bupropion Figure 30-2.Second-generation antidepressants
Figure 30-1. Structural relationships between various tricyclic antidepressants (TCAs). Figure 30-2. Second-generation antidepressants

-N CH3 N CH3 HO CH30 Mirtazapine Venlafaxine CH2CH2 0-CH2一CH2一N CH2一CH2一CH2 0 Nefazodone CH2、 NHCH3 CH CH2 Duloxetine Figure 30-3.Newer(third-generation)antidepressants 0-CH CH2 CH2CH2NHCH3 Fluoxetine Paroxetine NHCH3 Sertraline NC、 F3C CH2CH2CH2CH2OCH3 CH3 CH2CH2CH2N 0-CH2CH2NH2 Fluvoxamine Citalopram Figure 30-4.Selective serotonin reuptake inhibitors(SSRIs)
Figure 30-3. Newer (third-generation) antidepressants. Figure 30-4. Selective serotonin reuptake inhibitors (SSRIs)

CH2-CH2-NH一NH2 Phenelzine CH一CH-NH2 \/ CH2 Tranylcypromine Figure 30-5.Some monoamine oxidase inhibitors.Phenelzine is the hydrazide of phenylethylamine (see Figure 9-3),whereas tranylcypromine has a cyclopropyl amine side chain and closely resembles dextroamphetamine.These agents are unselective and produce an extremely long-lasting inhibition of the enzyme.Selegiline,which is partially selective for MAO-B,is shown in Figure 28-2. Pharmacokinetics A.TRICYCLIC ANTIDEPRESSANTS Most tricyclics are incompletely absorbed and undergo significant first-pass metabolism.As a result of high tissue protein binding and relatively high lipid solubility,volumes of distribution tend to be very large.Tricyclics are metabolized by two major routes:transformation of the tricyclic nucleus and alteration of the aliphatic side chain.Monodemethylation of tertiary amines leads to active metabolites such as desipramine and nortriptyline(which are themselves available as drugs;Figure 30-1). B.SECOND-GENERATION AND SUBSEQUENT ANTIDEPRESSANTS The pharmacokinetics of these drugs are similar to those of the TCAs(Table 30-1). Some have active metabolites.Trazodone and venlafaxine have short plasma half-lives,which mandates divided doses during the day when beginning treatment, although once-a-day dosing may be possible later.Extended-release forms of bupropion and venlafaxine allow for once-a-day dosing in some patients from the outset. C.SELECTIVE SEROTONIN REUPTAKE INHIBITORS The pharmacokinetic parameters of these drugs are summarized in Table 30-1. Fluoxetine is notable for the long half-life of its active metabolite,norfluoxetine(7-9 days at steady state).This long tip has allowed the introduction of a formulation for once-weekly dosing.Sertraline and paroxetine have pharmacokinetic parameters similar to those of tricyclics.Citalopram and fluvoxamine resemble fluoxetine
Figure 30-5. Some monoamine oxidase inhibitors. Phenelzine is the hydrazide of phenylethylamine (see Figure 9-3), whereas tranylcypromine has a cyclopropyl amine side chain and closely resembles dextroamphetamine. These agents are unselective and produce an extremely long-lasting inhibition of the enzyme. Selegiline, which is partially selective for MAO-B, is shown in Figure 28-2. Pharmacokinetics A. TRICYCLIC ANTIDEPRESSANTS Most tricyclics are incompletely absorbed and undergo significant first-pass metabolism. As a result of high tissue protein binding and relatively high lipid solubility, volumes of distribution tend to be very large. Tricyclics are metabolized by two major routes: transformation of the tricyclic nucleus and alteration of the aliphatic side chain. Monodemethylation of tertiary amines leads to active metabolites such as desipramine and nortriptyline (which are themselves available as drugs; Figure 30-1). B. SECOND-GENERATION AND SUBSEQUENT ANTIDEPRESSANTS The pharmacokinetics of these drugs are similar to those of the TCAs (Table 30-1). Some have active metabolites. Trazodone and venlafaxine have short plasma half-lives, which mandates divided doses during the day when beginning treatment, although once-a-day dosing may be possible later. Extended-release forms of bupropion and venlafaxine allow for once-a-day dosing in some patients from the outset. C. SELECTIVE SEROTONIN REUPTAKE INHIBITORS The pharmacokinetic parameters of these drugs are summarized in Table 30-1. Fluoxetine is notable for the long half-life of its active metabolite, norfluoxetine (7-9 days at steady state). This long t1/2 has allowed the introduction of a formulation for once-weekly dosing. Sertraline and paroxetine have pharmacokinetic parameters similar to those of tricyclics. Citalopram and fluvoxamine resemble fluoxetine
D.MAO INHIBITORS The monoamine oxidase inhibitors (MAOIs)are readily absorbed from the gastrointestinal tract.The hydrazide inhibitor phenelzine is acetylated in the liver and manifests differences in elimination,depending on the acetylation phenotype of the individual (see Chapter 4).However,inhibition of MAO persists even after these drugs (including selegiline)are no longer detectable in plasma.Therefore, conventional pharmacokinetic parameters (half-life,etc)are not very helpful in governing dosage.It is prudent to assume that the drug effect will persist for 7 days (tranylcypromine)to 2 or 3 weeks(phenelzine,selegiline)after discontinuance of the drug. Pharmacodynamics A ACTIONS OF ANTIDEPRESSANTS ON AMINE NEUROTRANSMITTERS The amine hypothesis was buttressed by studies on the mechanism of action of various types of antidepressant drugs.Tricyclics block the amine transporters(uptake pumps;Figure 30-6)known as the norepinephrine and serotonin transporters,NET and SERT,respectively.These transporters terminate amine neurotransmission (see Table 30-2 and Chapter 6).Blockade of these transporters presumably permits a longer sojourn of neurotransmitter in the intrasynaptic space at the receptor site.MAO inhibitors block a major intraneuronal degradative pathway for the amine neurotransmitters,which permits more amines to accumulate in presynaptic stores (Figure 30-6)and more to be released.Some of the second-generation antidepressants have similar strong effects on amine transporters,whereas others have only moderate or minimal effects on reuptake or metabolism.Countering this simple model of increased synaptic activity is increasing evidence of alterations in presynaptic regulation of neurotransmitter release.Presynaptic autoreceptors respond to increased synaptic transmitter by down-regulating transmitter synthesis and release. Furthermore,some (but not all)of these regulatory receptors may themselves be down-regulated.These changes occur on a slower time scale more in keeping with the clinically observed effects. Trazodone,nefazodone,and mirtazapine stand out as agents in which antagonism of subtypes of serotonin receptors(5-HT2A or 5-HT2c)may be important in their action. Mirtazapine is unique in including antagonism of a2 norepinephrine receptors as presumably contributing to its therapeutic effects.Bupropion has been found to alter the output of norepinephrine in humans following chronic administration through some as yet unidentified primary mechanism as well as occupying about 25%of dopamine uptake transporters(DAT)in the brain as revealed by positron emission tomography.(Since it has been shown that effective doses of SSRIs occupy 80%of serotonin uptake sites,the clinical relevance of 25%DAT occupancy is uncertain.) Thus,even the newest antidepressants can still be categorized as possibly working
D. MAO INHIBITORS The monoamine oxidase inhibitors (MAOIs) are readily absorbed from the gastrointestinal tract. The hydrazide inhibitor phenelzine is acetylated in the liver and manifests differences in elimination, depending on the acetylation phenotype of the individual (see Chapter 4). However, inhibition of MAO persists even after these drugs (including selegiline) are no longer detectable in plasma. Therefore, conventional pharmacokinetic parameters (half-life, etc) are not very helpful in governing dosage. It is prudent to assume that the drug effect will persist for 7 days (tranylcypromine) to 2 or 3 weeks (phenelzine, selegiline) after discontinuance of the drug. Pharmacodynamics A. ACTIONS OF ANTIDEPRESSANTS ON AMINE NEUROTRANSMITTERS The amine hypothesis was buttressed by studies on the mechanism of action of various types of antidepressant drugs. Tricyclics block the amine transporters (uptake pumps; Figure 30-6) known as the norepinephrine and serotonin transporters, NET and SERT, respectively. These transporters terminate amine neurotransmission (see Table 30-2 and Chapter 6). Blockade of these transporters presumably permits a longer sojourn of neurotransmitter in the intrasynaptic space at the receptor site. MAO inhibitors block a major intraneuronal degradative pathway for the amine neurotransmitters, which permits more amines to accumulate in presynaptic stores (Figure 30-6) and more to be released. Some of the second-generation antidepressants have similar strong effects on amine transporters, whereas others have only moderate or minimal effects on reuptake or metabolism. Countering this simple model of increased synaptic activity is increasing evidence of alterations in presynaptic regulation of neurotransmitter release. Presynaptic autoreceptors respond to increased synaptic transmitter by down-regulating transmitter synthesis and release. Furthermore, some (but not all) of these regulatory receptors may themselves be down-regulated. These changes occur on a slower time scale more in keeping with the clinically observed effects. Trazodone, nefazodone, and mirtazapine stand out as agents in which antagonism of subtypes of serotonin receptors (5-HT2A or 5-HT2C) may be important in their action. Mirtazapine is unique in including antagonism of a2 norepinephrine receptors as presumably contributing to its therapeutic effects. Bupropion has been found to alter the output of norepinephrine in humans following chronic administration through some as yet unidentified primary mechanism as well as occupying about 25% of dopamine uptake transporters (DAT) in the brain as revealed by positron emission tomography. (Since it has been shown that effective doses of SSRIs occupy 80% of serotonin uptake sites, the clinical relevance of 25% DAT occupancy is uncertain.) Thus, even the newest antidepressants can still be categorized as possibly working

through serotonergic and noradrenergic effects with the additional possibility of a role for dopamine.Increased synaptic dopamine has often been invoked as relevant to the efficacy of MAOIs. B.RECEPTOR AND POSTRECEPTOR EFFECTS Considerable attention has been paid to the long-term postsynaptic effects of increased neurotransmitters in the synapses.In tests of postsynaptic effects,especially of the tricyclics,cAMP concentrations have consistently decreased rather than increased.In addition,the number of receptors for the neurotransmitters can decrease over the same time course as clinical improvement in patients.Thus,the initial increase in neurotransmitter seen with some antidepressants appears to produce,over time,a compensatory decrease in receptor activity,ie,down-regulation of certain postsynaptic as well as presynaptic receptors. It has long been thought that enhanced serotonergic transmission,albeit mediated through diverse mechanisms,might be a common effect of antidepressants even without an increase in synaptic serotonin.Moreover,selective antagonism of either norepinephrine or serotonin receptors as opposed to that of the 5-HT transporter may lead to enhanced extracellular serotonin due to the complex manner in which these neurotransmitters are regulated. Most recently,long-term intracellular changes involving phosphorylation of various regulatory elements,including those within the nucleus,have been implicated as relevant to antidepressant action.It is possible that effects on certain neurotrophic factors%factors critical to sustained survival and function of neurons in the adult nervous system%may be central to the actions of antidepressants. Clinical studies have indirectly tested the relevance of findings from animals for norepinephrine or serotonin function.The approach has been to reduce the amino acid precursor of serotonin,tryptophan,in the diet and,by implication,the amount of available neurotransmitter in the brain,since tryptophan availability can be rate-limiting in the formation of serotonin.Severely tryptophan-depleted diets reduce plasma tryptophan and acutely reverse antidepressant responses to SSRIs but not to NET inhibitors.Similarly,depletion of the norepinephrine amino acid precursor tyrosine can reverse antidepressant effects of the relatively selective NET inhibitor, desipramine.These findings support the hypothesis that enhanced serotonin and norepinephrine throughput is necessary for the antidepressant actions of the respective transporter inhibitors.However,tryptophan depletion does not consistently worsen the condition of unmedicated depressed patients.Thus,there is still no clear relationship between serotonin and depression or antidepressant mechanisms in general. C.EFFECTS OF SPECIFIC ANTIDEPRESSANTS
through serotonergic and noradrenergic effects with the additional possibility of a role for dopamine. Increased synaptic dopamine has often been invoked as relevant to the efficacy of MAOIs. B. RECEPTOR AND POSTRECEPTOR EFFECTS Considerable attention has been paid to the long-term postsynaptic effects of increased neurotransmitters in the synapses. In tests of postsynaptic effects, especially of the tricyclics, cAMP concentrations have consistently decreased rather than increased. In addition, the number of receptors for the neurotransmitters can decrease over the same time course as clinical improvement in patients. Thus, the initial increase in neurotransmitter seen with some antidepressants appears to produce, over time, a compensatory decrease in receptor activity, ie, down-regulation of certain postsynaptic as well as presynaptic receptors. It has long been thought that enhanced serotonergic transmission, albeit mediated through diverse mechanisms, might be a common effect of antidepressants even without an increase in synaptic serotonin. Moreover, selective antagonism of either norepinephrine or serotonin receptors as opposed to that of the 5-HT transporter may lead to enhanced extracellular serotonin due to the complex manner in which these neurotransmitters are regulated. Most recently, long-term intracellular changes involving phosphorylation of various regulatory elements, including those within the nucleus, have been implicated as relevant to antidepressant action. It is possible that effects on certain neurotrophic factors¾factors critical to sustained survival and function of neurons in the adult nervous system¾may be central to the actions of antidepressants. Clinical studies have indirectly tested the relevance of findings from animals for norepinephrine or serotonin function. The approach has been to reduce the amino acid precursor of serotonin, tryptophan, in the diet and, by implication, the amount of available neurotransmitter in the brain, since tryptophan availability can be rate-limiting in the formation of serotonin. Severely tryptophan-depleted diets reduce plasma tryptophan and acutely reverse antidepressant responses to SSRIs but not to NET inhibitors. Similarly, depletion of the norepinephrine amino acid precursor tyrosine can reverse antidepressant effects of the relatively selective NET inhibitor, desipramine. These findings support the hypothesis that enhanced serotonin and norepinephrine throughput is necessary for the antidepressant actions of the respective transporter inhibitors. However, tryptophan depletion does not consistently worsen the condition of unmedicated depressed patients. Thus, there is still no clear relationship between serotonin and depression or antidepressant mechanisms in general. C. EFFECTS OF SPECIFIC ANTIDEPRESSANTS

1.Tricyclics The first-generation antidepressants demonstrate varying degrees of selectivity for the reuptake pumps for norepinephrine and serotonin(Table 30-2)but selectivity is much lower than for the SSRIs.They also have numerous autonomic actions,as described below under Adverse Effects. 2.Second-generation agents Amoxapine is a metabolite of the antipsychotic drug loxapine and retains some of its antipsychotic action and dopamine receptor antagonism (see Chapter 29).A combination of antidepressant and antipsychotic actions might make it a suitable drug for depression in psychotic patients.However, the dopamine antagonism may cause akathisia, parkinsonism, amenorrhea-galactorrhea syndrome,and perhaps tardive dyskinesia. Maprotiline (a tetracyclic drug)is most like desipramine in terms of its potent norepinephrine uptake inhibition.Like desipramine,it has fewer sedative and antimuscarinic actions than the older tricyclics. Clinical experience with trazodone has indicated unpredictable efficacy for depression, although it has proved very useful as a hypnotic,sometimes being combined with MAOIs,which disturb sleep. 3.Subsequent non-SSRI agents%Four antidepressants%nefazodone,venlafaxine, duloxetine,and mirtazapine%are all related to earlier agents in either structure or mechanism of action.Nefazodone is closely related to trazodone but is less sedating. It produces fewer adverse sexual effects than the SSRIs (see below)but is a potent inhibitor of CYP3A4.(Fluvoxamine causes the same inhibition of CYP3A4.) Venlafaxine is a potent inhibitor of serotonin transport and a weaker inhibitor of norepinephrine transport.At lower therapeutic doses,venlafaxine behaves like an SSRI.At high doses (more than 225 mg/d),it produces mild to moderate increases of heart rate and blood pressure attributable to norepinephrine transporter inhibition. Doses in the range of 225 mg/d or more may confer broader therapeutic effects than SSRIs,but titration up to these doses is needed to control adverse effects. Mirtazapine is a potent antihistaminic with greater sedating effects than the other second-and third-generation antidepressants.Its use is also more likely to be associated with weight gain.The hypothesized mechanism of action of mirtazapine combines 5-HT2 receptor and a-adrenoceptor antagonism and,if established in humans,would be unique among available drugs.Thus,mirtazapine may prove beneficial in patients who can tolerate its sedative effects and do not respond well to SSRIs or cannot tolerate their sexual adverse effects. 4.Selective serotonin reuptake inhibitors%These drugs achieve high ratios of SERT versus NET inhibition of 300 to 7000 (Table 30-2).Fluoxetine was the first SSRI to reach general clinical use.Paroxetine and sertraline differ mainly in having
1. Tricyclics The first-generation antidepressants demonstrate varying degrees of selectivity for the reuptake pumps for norepinephrine and serotonin (Table 30-2) but selectivity is much lower than for the SSRIs. They also have numerous autonomic actions, as described below under Adverse Effects. 2. Second-generation agents Amoxapine is a metabolite of the antipsychotic drug loxapine and retains some of its antipsychotic action and dopamine receptor antagonism (see Chapter 29). A combination of antidepressant and antipsychotic actions might make it a suitable drug for depression in psychotic patients. However, the dopamine antagonism may cause akathisia, parkinsonism, amenorrhea-galactorrhea syndrome, and perhaps tardive dyskinesia. Maprotiline (a tetracyclic drug) is most like desipramine in terms of its potent norepinephrine uptake inhibition. Like desipramine, it has fewer sedative and antimuscarinic actions than the older tricyclics. Clinical experience with trazodone has indicated unpredictable efficacy for depression, although it has proved very useful as a hypnotic, sometimes being combined with MAOIs, which disturb sleep. 3. Subsequent non-SSRI agents¾ Four antidepressants¾nefazodone, venlafaxine, duloxetine, and mirtazapine¾are all related to earlier agents in either structure or mechanism of action. Nefazodone is closely related to trazodone but is less sedating. It produces fewer adverse sexual effects than the SSRIs (see below) but is a potent inhibitor of CYP3A4. (Fluvoxamine causes the same inhibition of CYP3A4.) Venlafaxine is a potent inhibitor of serotonin transport and a weaker inhibitor of norepinephrine transport. At lower therapeutic doses, venlafaxine behaves like an SSRI. At high doses (more than 225 mg/d), it produces mild to moderate increases of heart rate and blood pressure attributable to norepinephrine transporter inhibition. Doses in the range of 225 mg/d or more may confer broader therapeutic effects than SSRIs, but titration up to these doses is needed to control adverse effects. Mirtazapine is a potent antihistaminic with greater sedating effects than the other second- and third-generation antidepressants. Its use is also more likely to be associated with weight gain. The hypothesized mechanism of action of mirtazapine combines 5-HT2 receptor and a-adrenoceptor antagonism and, if established in humans, would be unique among available drugs. Thus, mirtazapine may prove beneficial in patients who can tolerate its sedative effects and do not respond well to SSRIs or cannot tolerate their sexual adverse effects. 4. Selective serotonin reuptake inhibitors¾ These drugs achieve high ratios of SERT versus NET inhibition of 300 to 7000 (Table 30-2). Fluoxetine was the first SSRI to reach general clinical use. Paroxetine and sertraline differ mainly in having

shorter half-lives and different potencies as inhibitors of specific P450 isoenzymes. Racemic citalopram and (S)-citalopram(escitalopram),the most selective SSRIs of all have achieved very widespread use.Although the SSRIs have not been shown to be more effective overall than prior drugs,they lack many of the toxicities of the tricyclic and heterocyclic antidepressants.Thus,patient acceptance has been high despite their own adverse effects. 5.MAO inhibitors MAO-A (isoform A)is the amine oxidase primarily responsible for norepinephrine,serotonin,and tyramine metabolism.MAO-B is more selective for dopamine.The irreversible inhibitors available in the USA are nonselective and at the doses used block both forms of the enzyme.Irreversible block of MAO,characteristic of the older MAO inhibitors,allows significant accumulation of tyramine and loss of the first-pass metabolism that protects against tyramine in foods(see Adverse Effects). Because they result in replacement of the normal transmitter(norepinephrine)stored in noradrenergic nerve terminal vesicles with a false transmitter (octopamine),they may cause significant hypotension. T 5HT1D.2A VAT VAT MAO-A 02 Ca2+ 5HT1A.1D Figure 30-6 Schematic diagram showing some of the potential sites of action of antidepressant drugs.The primary neuron is shown as releasing a transmitter amine (NT).A modulating neuron may release a second transmitter(NTx),regulating the activity of the primary neuron.The most consistent observed effect of the antidepressants(other than MAO inhibitors)is inhibition of the reuptake transporters (T)for norepinephrine or serotonin.The MAO inhibitors increase the vesicular stores of both NE and 5-HT.Other direct or indirect effects include initial increase in activation of pre-and postsynaptic receptors and subsequent desensitization or down-regulation of transmitter synthesis from an amino acid(AA),receptor numbers, or postreceptor mechanisms.Desensitization resulting from antidepressant use has
shorter half-lives and different potencies as inhibitors of specific P450 isoenzymes. Racemic citalopram and (S)-citalopram (escitalopram), the most selective SSRIs of all, have achieved very widespread use. Although the SSRIs have not been shown to be more effective overall than prior drugs, they lack many of the toxicities of the tricyclic and heterocyclic antidepressants. Thus, patient acceptance has been high despite their own adverse effects. 5. MAO inhibitors MAO-A (isoform A) is the amine oxidase primarily responsible for norepinephrine, serotonin, and tyramine metabolism. MAO-B is more selective for dopamine. The irreversible inhibitors available in the USA are nonselective and at the doses used block both forms of the enzyme. Irreversible block of MAO, characteristic of the older MAO inhibitors, allows significant accumulation of tyramine and loss of the first-pass metabolism that protects against tyramine in foods (see Adverse Effects). Because they result in replacement of the normal transmitter (norepinephrine) stored in noradrenergic nerve terminal vesicles with a false transmitter (octopamine), they may cause significant hypotension. Figure 30-6 Schematic diagram showing some of the potential sites of action of antidepressant drugs. The primary neuron is shown as releasing a transmitter amine (NT). A modulating neuron may release a second transmitter (NTx), regulating the activity of the primary neuron. The most consistent observed effect of the antidepressants (other than MAO inhibitors) is inhibition of the reuptake transporters (T) for norepinephrine or serotonin. The MAO inhibitors increase the vesicular stores of both NE and 5-HT. Other direct or indirect effects include initial increase in activation of pre- and postsynaptic receptors and subsequent desensitization or down-regulation of transmitter synthesis from an amino acid (AA), receptor numbers, or postreceptor mechanisms. Desensitization resulting from antidepressant use has