
Pharmacologic Management of Parkinsonism Other Movement Disorders Michael J.Aminoff,MD,DSc,FRCP INTRODUCTION Several types of abnormal movement are recognized.Tremor consists of a rhythmic oscillatory movement around a joint and is best characterized by its relation to activity. Tremor at rest is characteristic of parkinsonism,when it is often associated with rigidity and an impairment of voluntary activity.Tremor may occur during maintenance of sustained posture(postural tremor)or during movement(intention tremor).A conspicuous postural tremor is the cardinal feature of benign essential or familial tremor.Intention tremor occurs in patients with a lesion of the brainstem or cerebellum,especially when the superior cerebellar peduncle is involved,and may also occur as a manifestation of toxicity from alcohol or certain other drugs. Chorea consists of irregular,unpredictable,involuntary muscle jerks that occur in different parts of the body and impair voluntary activity.In some instances,the proximal muscles of the limbs are most severely affected,and because the abnormal movements are then particularly violent,the term ballismus has been used to describe them.Chorea may be hereditary or may occur as a complication of a number of general medical disorders and of therapy with certain drugs. Abnormal movements may be slow and writhing in character(athetosis)and in some instances are so sustained that they are more properly regarded as abnormal postures (dystonia).Athetosis or dystonia may occur with perinatal brain damage,with focal or generalized cerebral lesions,as an acute complication of certain drugs,as an accompaniment of diverse neurologic disorders,or as an isolated inherited phenomenon of uncertain cause known as idiopathic torsion dystonia or dystonia musculorum deformans.Its physiologic basis is uncertain,and treatment is unsatisfactory. Tics are sudden coordinated abnormal movements that tend to occur repetitively, particularly about the face and head,especially in children,and can be suppressed voluntarily for short periods of time.Common tics include repetitive sniffing or shoulder shrugging.Tics may be single or multiple and transient or chronic.Gilles de la Tourette's syndrome is characterized by chronic multiple tics;its pharmacologic management is discussed at the end of this chapter. Many of the movement disorders have been attributed to disturbances of the basal ganglia,but the precise function of these anatomic structures is not yet fully understood,and it is not possible to relate individual symptoms to involvement at specific sites
Pharmacologic Management of Parkinsonism & Other Movement Disorders Michael J. Aminof , MD, DSc, FRCP INTRODUCTION Several types of abnormal movement are recognized. Tremor consists of a rhythmic oscillatory movement around a joint and is best characterized by its relation to activity. Tremor at rest is characteristic of parkinsonism, when it is often associated with rigidity and an impairment of voluntary activity. Tremor may occur during maintenance of sustained posture (postural tremor) or during movement (intention tremor). A conspicuous postural tremor is the cardinal feature of benign essential or familial tremor. Intention tremor occurs in patients with a lesion of the brainstem or cerebellum, especially when the superior cerebellar peduncle is involved, and may also occur as a manifestation of toxicity from alcohol or certain other drugs. Chorea consists of irregular, unpredictable, involuntary muscle jerks that occur in different parts of the body and impair voluntary activity. In some instances, the proximal muscles of the limbs are most severely affected, and because the abnormal movements are then particularly violent, the term ballismus has been used to describe them. Chorea may be hereditary or may occur as a complication of a number of general medical disorders and of therapy with certain drugs. Abnormal movements may be slow and writhing in character (athetosis) and in some instances are so sustained that they are more properly regarded as abnormal postures (dystonia). Athetosis or dystonia may occur with perinatal brain damage, with focal or generalized cerebral lesions, as an acute complication of certain drugs, as an accompaniment of diverse neurologic disorders, or as an isolated inherited phenomenon of uncertain cause known as idiopathic torsion dystonia or dystonia musculorum deformans. Its physiologic basis is uncertain, and treatment is unsatisfactory. Tics are sudden coordinated abnormal movements that tend to occur repetitively, particularly about the face and head, especially in children, and can be suppressed voluntarily for short periods of time. Common tics include repetitive sniffing or shoulder shrugging. Tics may be single or multiple and transient or chronic. Gilles de la Tourette's syndrome is characterized by chronic multiple tics; its pharmacologic management is discussed at the end of this chapter. Many of the movement disorders have been attributed to disturbances of the basal ganglia, but the precise function of these anatomic structures is not yet fully understood, and it is not possible to relate individual symptoms to involvement at specific sites
PARKINSONISM (PARALYSIS AGITANS) INTRODUCTION Parkinsonism is characterized by a combination of rigidity,bradykinesia,tremor,and postural instability that can occur for a variety of reasons but is usually idiopathic. The pathophysiologic basis of the idiopathic disorder may relate to exposure to some unrecognized neurotoxin or to the occurrence of oxidation reactions with the generation of free radicals.Studies in twins suggest that genetic factors may also be important,especially when the disease occurs in patients under age 50.Parkinson's disease is generally progressive,leading to increasing disability unless effective treatment is provided. The normally high concentration of dopamine in the basal ganglia of the brain is reduced in parkinsonism,and pharmacologic attempts to restore dopaminergic activity with levodopa and dopamine agonists have been successful in alleviating many of the clinical features of the disorder.An alternative but complementary approach has been to restore the normal balance of cholinergic and dopaminergic influences on the basal ganglia with antimuscarinic drugs.The pathophysiologic basis for these therapies is that in idiopathic parkinsonism,dopaminergic neurons in the substantia nigra that normally inhibit the output of GABAergic cells in the corpus striatum are lost(Figure 28-1).(In contrast,Huntington's chorea involves the loss of some cholinergic neurons and an even greater loss of the GABAergic cells that exit the corpus striatum.) Drugs that induce parkinsonian syndromes either are dopamine receptor antagonists or lead to the destruction of the dopaminergic nigrostriatal neurons (eg, 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine [MPTP];see below). Normal Substantia Corpus nigra striatum ⊙ Dopamine Acetyl- GABA choline L Parkinsonism L Huntington's disease
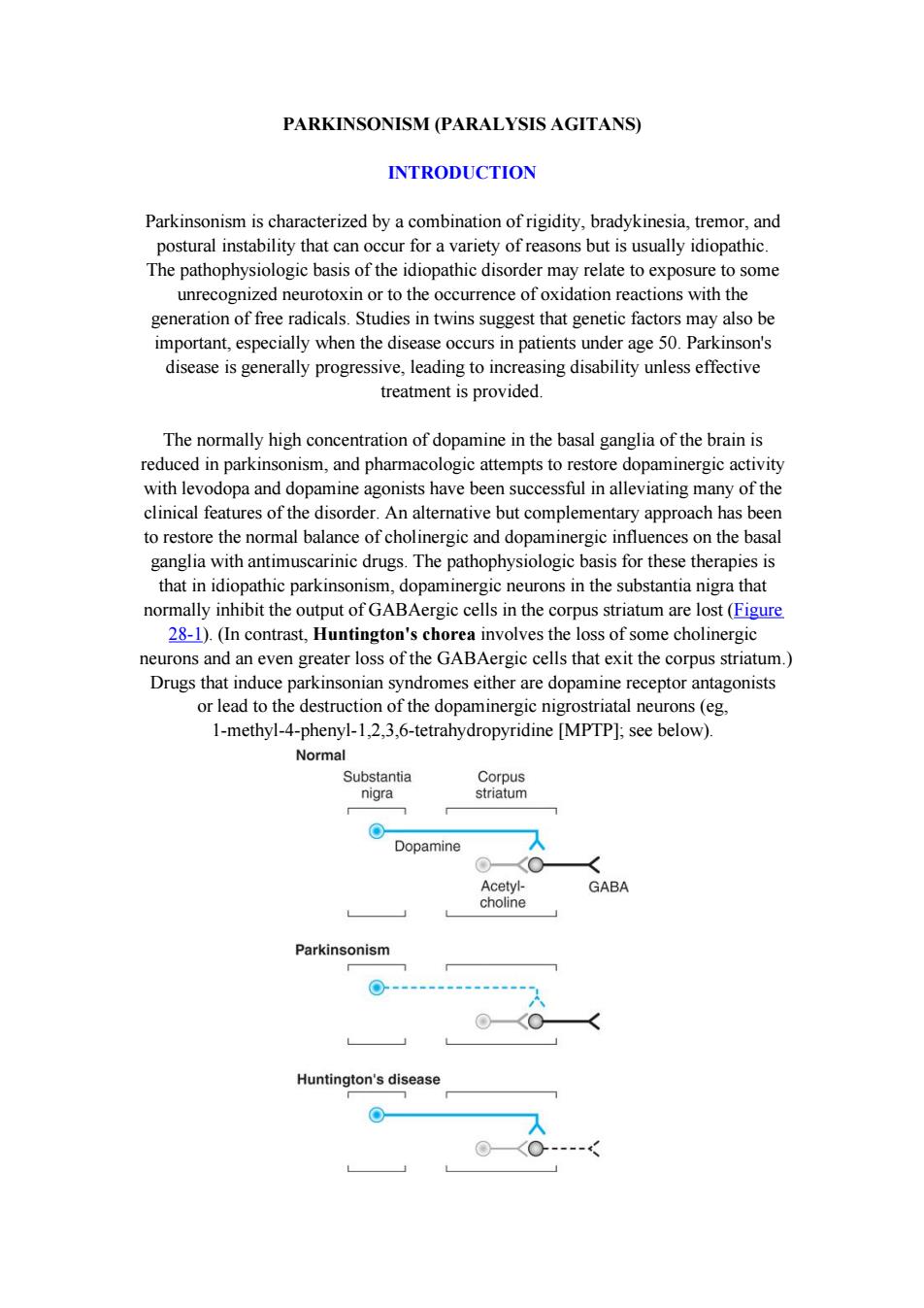
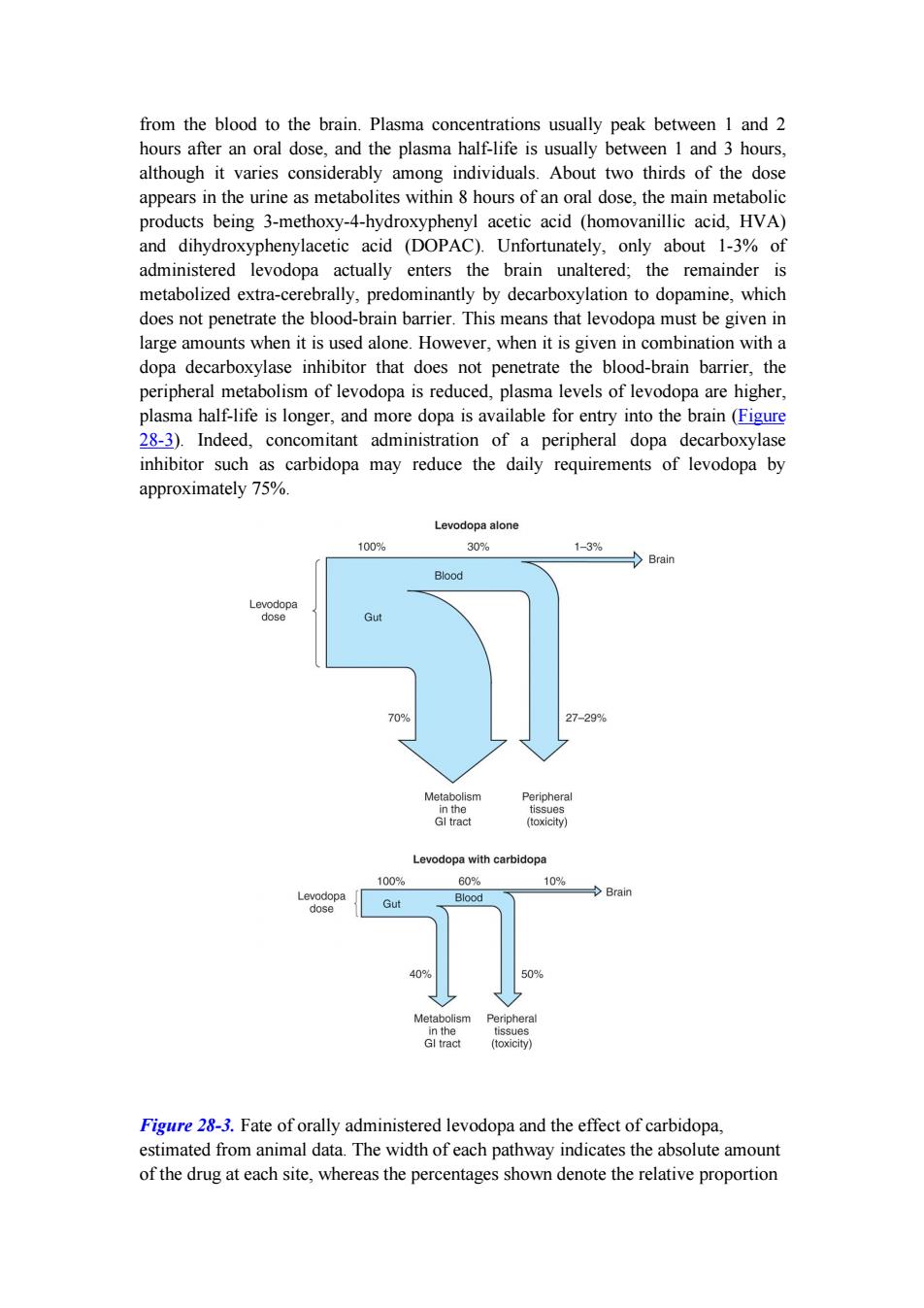
PARKINSONISM (PARALYSIS AGITANS) INTRODUCTION Parkinsonism is characterized by a combination of rigidity, bradykinesia, tremor, and postural instability that can occur for a variety of reasons but is usually idiopathic. The pathophysiologic basis of the idiopathic disorder may relate to exposure to some unrecognized neurotoxin or to the occurrence of oxidation reactions with the generation of free radicals. Studies in twins suggest that genetic factors may also be important, especially when the disease occurs in patients under age 50. Parkinson's disease is generally progressive, leading to increasing disability unless effective treatment is provided. The normally high concentration of dopamine in the basal ganglia of the brain is reduced in parkinsonism, and pharmacologic attempts to restore dopaminergic activity with levodopa and dopamine agonists have been successful in alleviating many of the clinical features of the disorder. An alternative but complementary approach has been to restore the normal balance of cholinergic and dopaminergic influences on the basal ganglia with antimuscarinic drugs. The pathophysiologic basis for these therapies is that in idiopathic parkinsonism, dopaminergic neurons in the substantia nigra that normally inhibit the output of GABAergic cells in the corpus striatum are lost (Figure 28-1). (In contrast, Huntington's chorea involves the loss of some cholinergic neurons and an even greater loss of the GABAergic cells that exit the corpus striatum.) Drugs that induce parkinsonian syndromes either are dopamine receptor antagonists or lead to the destruction of the dopaminergic nigrostriatal neurons (eg, 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine [MPTP]; see below)
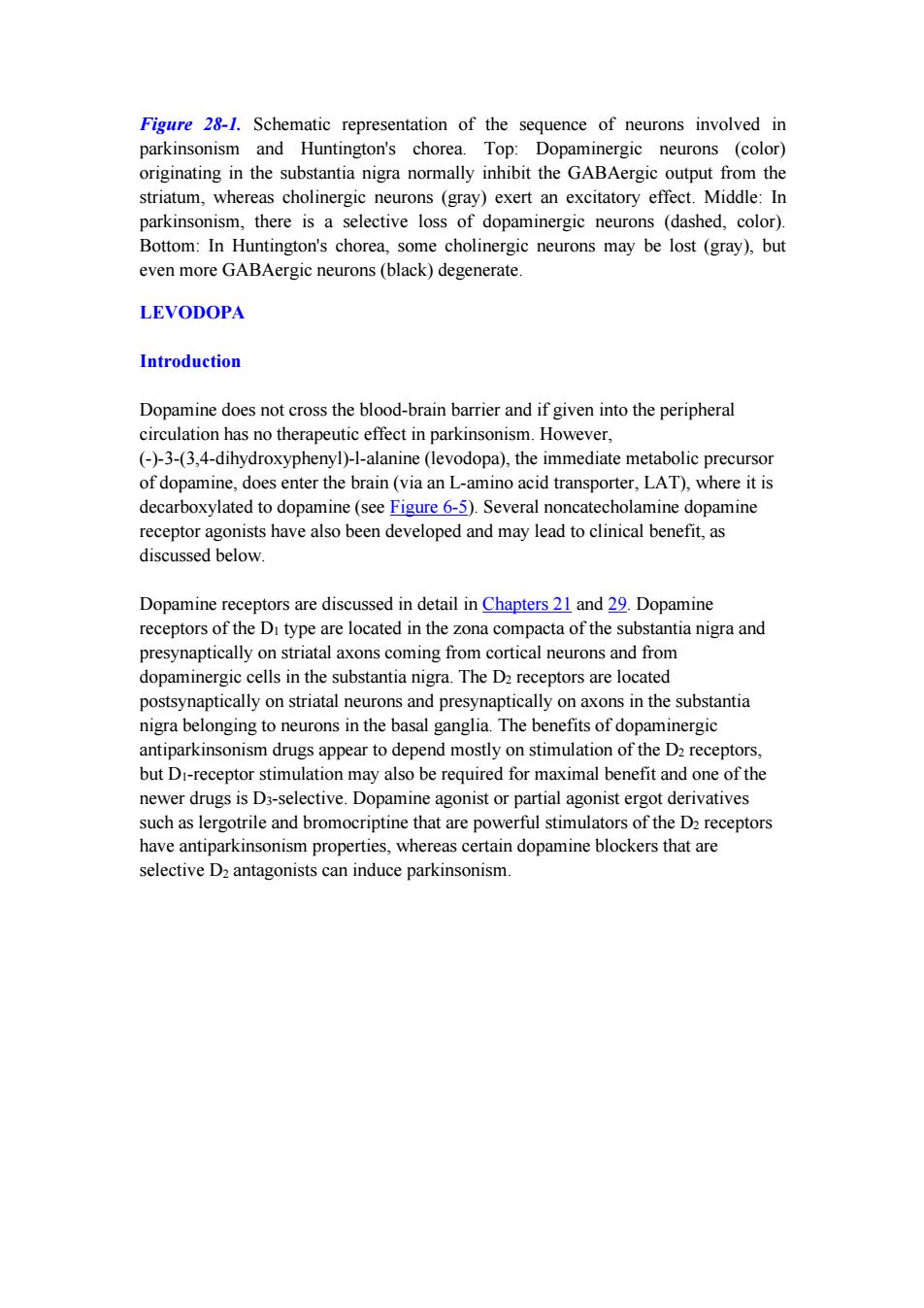
Figure 28-1.Schematic representation of the sequence of neurons involved in parkinsonism and Huntington's chorea.Top:Dopaminergic neurons (color) originating in the substantia nigra normally inhibit the GABAergic output from the striatum,whereas cholinergic neurons (gray)exert an excitatory effect.Middle:In parkinsonism,there is a selective loss of dopaminergic neurons (dashed,color). Bottom:In Huntington's chorea,some cholinergic neurons may be lost (gray),but even more GABAergic neurons(black)degenerate. LEVODOPA Introduction Dopamine does not cross the blood-brain barrier and if given into the peripheral circulation has no therapeutic effect in parkinsonism.However, (-)-3-(3,4-dihydroxyphenyl)-1-alanine (levodopa),the immediate metabolic precursor of dopamine,does enter the brain(via an L-amino acid transporter,LAT),where it is decarboxylated to dopamine(see Figure 6-5).Several noncatecholamine dopamine receptor agonists have also been developed and may lead to clinical benefit,as discussed below. Dopamine receptors are discussed in detail in Chapters 21 and 29.Dopamine receptors of the Di type are located in the zona compacta of the substantia nigra and presynaptically on striatal axons coming from cortical neurons and from dopaminergic cells in the substantia nigra.The D2 receptors are located postsynaptically on striatal neurons and presynaptically on axons in the substantia nigra belonging to neurons in the basal ganglia.The benefits of dopaminergic antiparkinsonism drugs appear to depend mostly on stimulation of the D2 receptors, but Di-receptor stimulation may also be required for maximal benefit and one of the newer drugs is D3-selective.Dopamine agonist or partial agonist ergot derivatives such as lergotrile and bromocriptine that are powerful stimulators of the D2 receptors have antiparkinsonism properties,whereas certain dopamine blockers that are selective D2 antagonists can induce parkinsonism
Figure 28-1. Schematic representation of the sequence of neurons involved in parkinsonism and Huntington's chorea. Top: Dopaminergic neurons (color) originating in the substantia nigra normally inhibit the GABAergic output from the striatum, whereas cholinergic neurons (gray) exert an excitatory effect. Middle: In parkinsonism, there is a selective loss of dopaminergic neurons (dashed, color). Bottom: In Huntington's chorea, some cholinergic neurons may be lost (gray), but even more GABAergic neurons (black) degenerate. LEVODOPA Introduction Dopamine does not cross the blood-brain barrier and if given into the peripheral circulation has no therapeutic effect in parkinsonism. However, (-)-3-(3,4-dihydroxyphenyl)-l-alanine (levodopa), the immediate metabolic precursor of dopamine, does enter the brain (via an L-amino acid transporter, LAT), where it is decarboxylated to dopamine (see Figure 6-5). Several noncatecholamine dopamine receptor agonists have also been developed and may lead to clinical benefit, as discussed below. Dopamine receptors are discussed in detail in Chapters 21 and 29. Dopamine receptors of the D1 type are located in the zona compacta of the substantia nigra and presynaptically on striatal axons coming from cortical neurons and from dopaminergic cells in the substantia nigra. The D2 receptors are located postsynaptically on striatal neurons and presynaptically on axons in the substantia nigra belonging to neurons in the basal ganglia. The benefits of dopaminergic antiparkinsonism drugs appear to depend mostly on stimulation of the D2 receptors, but D1-receptor stimulation may also be required for maximal benefit and one of the newer drugs is D3-selective. Dopamine agonist or partial agonist ergot derivatives such as lergotrile and bromocriptine that are powerful stimulators of the D2 receptors have antiparkinsonism properties, whereas certain dopamine blockers that are selective D2 antagonists can induce parkinsonism
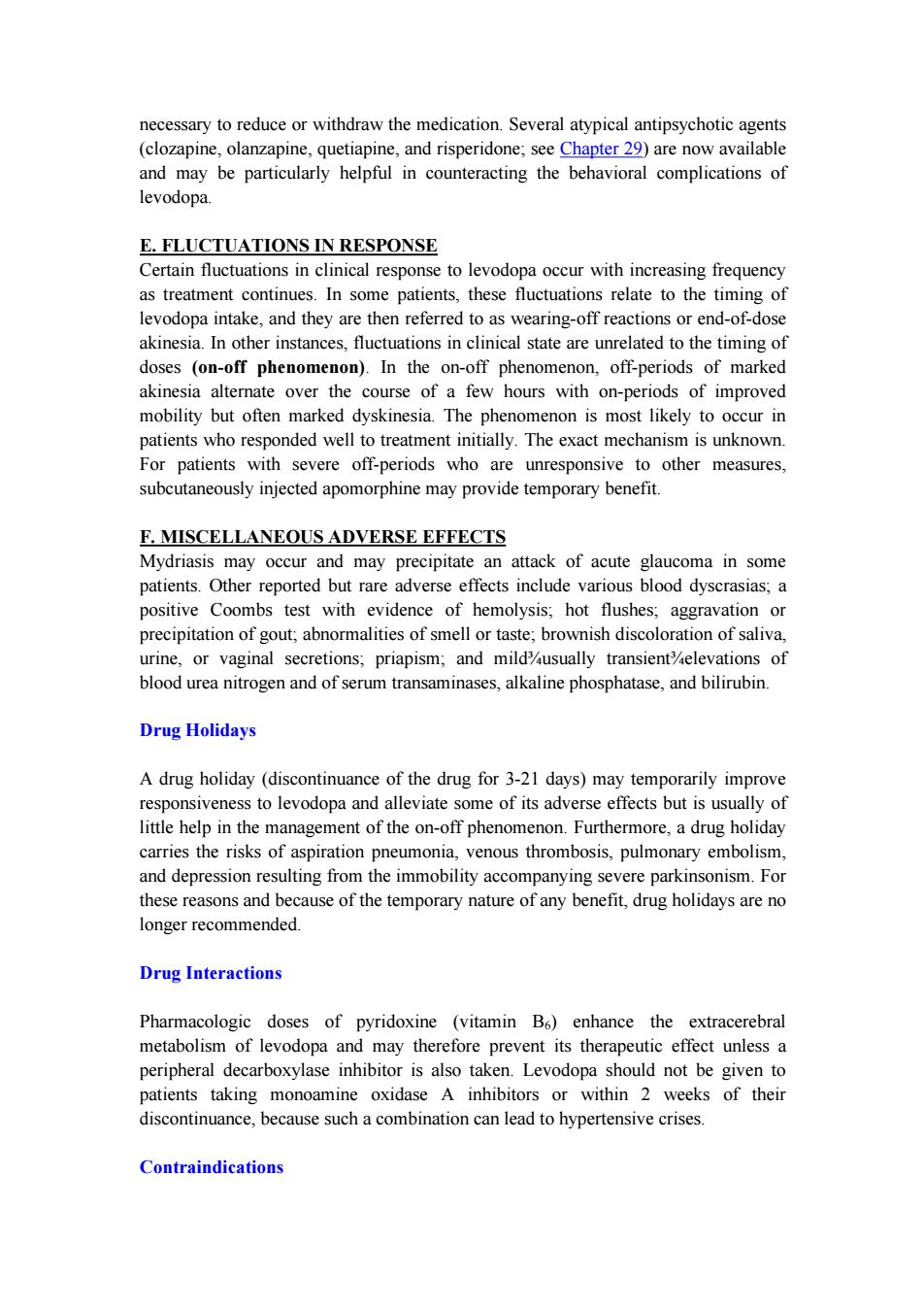
OH NH Tyrosine L-Amino acid decarboxylase Metyrosine Tyrosine hydroxylase OH C=0 HO C-NH H Dopa Tyramine C00H Dopa decarboxylase Dopamine HO B-hydroxylase HO 0 H N-Methyl- Dopamine HO -NH transterase Dopamine B-hydroxylase Octopamine Hydroxylase (from liver) 0 Epinine Norepinephrine Phenylethanolamine-N-methyltransferase Phenylamine- B-hydroxylase HO H Epinephrine Figure 6-5.Biosynthesis of catecholamines.The rate-limiting step,conversion of tyrosine to dopa,can be inhibited by metyrosine(a-methyltyrosine).The alternative pathways shown by the dashed arrows have not been found to be of physiologic significance in humans.However,tyramine and octopamine may accumulate in patients treated with monoamine oxidase inhibitors.(Reproduced,with permission, from Greenspan FS,Gardner DG (editors):Basic and Clinical Endocrinology,7th ed. McGraw-Hill,2003.) Chemistry As discussed in Chapter 6,dopa is the amino acid precursor of dopamine and norepinephrine.Its structure is shown in Figure 28-2.Levodopa is the levorotatory stereoisomer of dopa
Figure 6-5. Biosynthesis of catecholamines. The rate-limiting step, conversion of tyrosine to dopa, can be inhibited by metyrosine (a-methyltyrosine). The alternative pathways shown by the dashed arrows have not been found to be of physiologic significance in humans. However, tyramine and octopamine may accumulate in patients treated with monoamine oxidase inhibitors. (Reproduced, with permission, from Greenspan FS, Gardner DG (editors): Basic and Clinical Endocrinology, 7th ed. McGraw-Hill, 2003.) Chemistry As discussed in Chapter 6, dopa is the amino acid precursor of dopamine and norepinephrine. Its structure is shown in Figure 28-2. Levodopa is the levorotatory stereoisomer of dopa
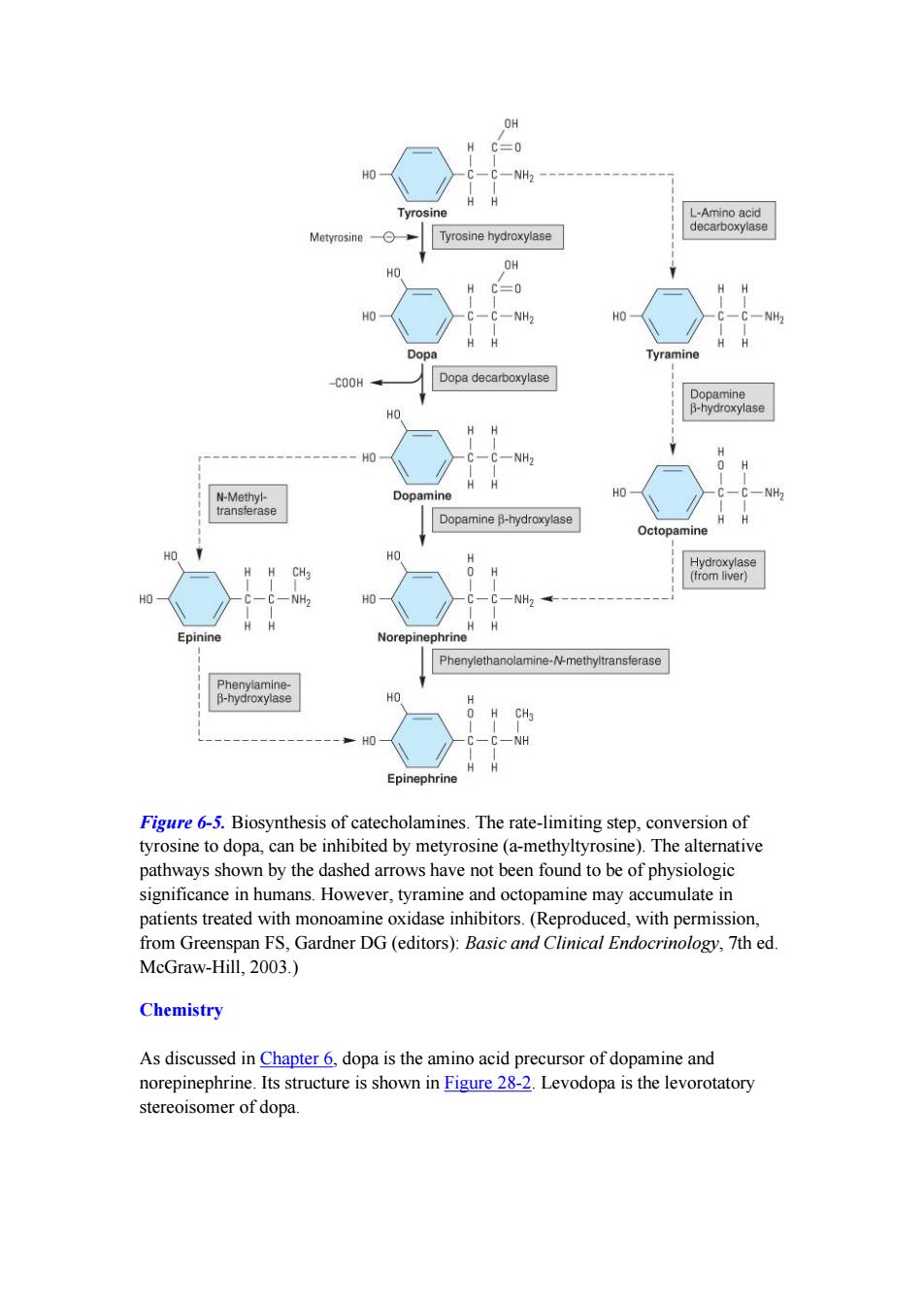
HO CH2-CH-COOH NH2 HO Dihydroxyphenylalanine (dopa) CH3 HO CH2-C-COOH NH-NH2 HO Carbidopa CH3 CH2一CH一N一CH2一C≡CH CH3 Selegiline C≡N CH2CH3 02N CH=C一C一N ∥ CH2CH3 0 HO OH Entacapone Figure 28-2.Some drugs used in the treatment of parkinsonism. Pharmacokinetics Levodopa is rapidly absorbed from the small intestine,but its absorption depends on the rate of gastric emptying and the pH of the gastric contents.Ingestion of food delays the appearance of levodopa in the plasma.Moreover,certain amino acids from ingested food can compete with the drug for absorption from the gut and for transport
Figure 28-2. Some drugs used in the treatment of parkinsonism. Pharmacokinetics Levodopa is rapidly absorbed from the small intestine, but its absorption depends on the rate of gastric emptying and the pH of the gastric contents. Ingestion of food delays the appearance of levodopa in the plasma. Moreover, certain amino acids from ingested food can compete with the drug for absorption from the gut and for transport
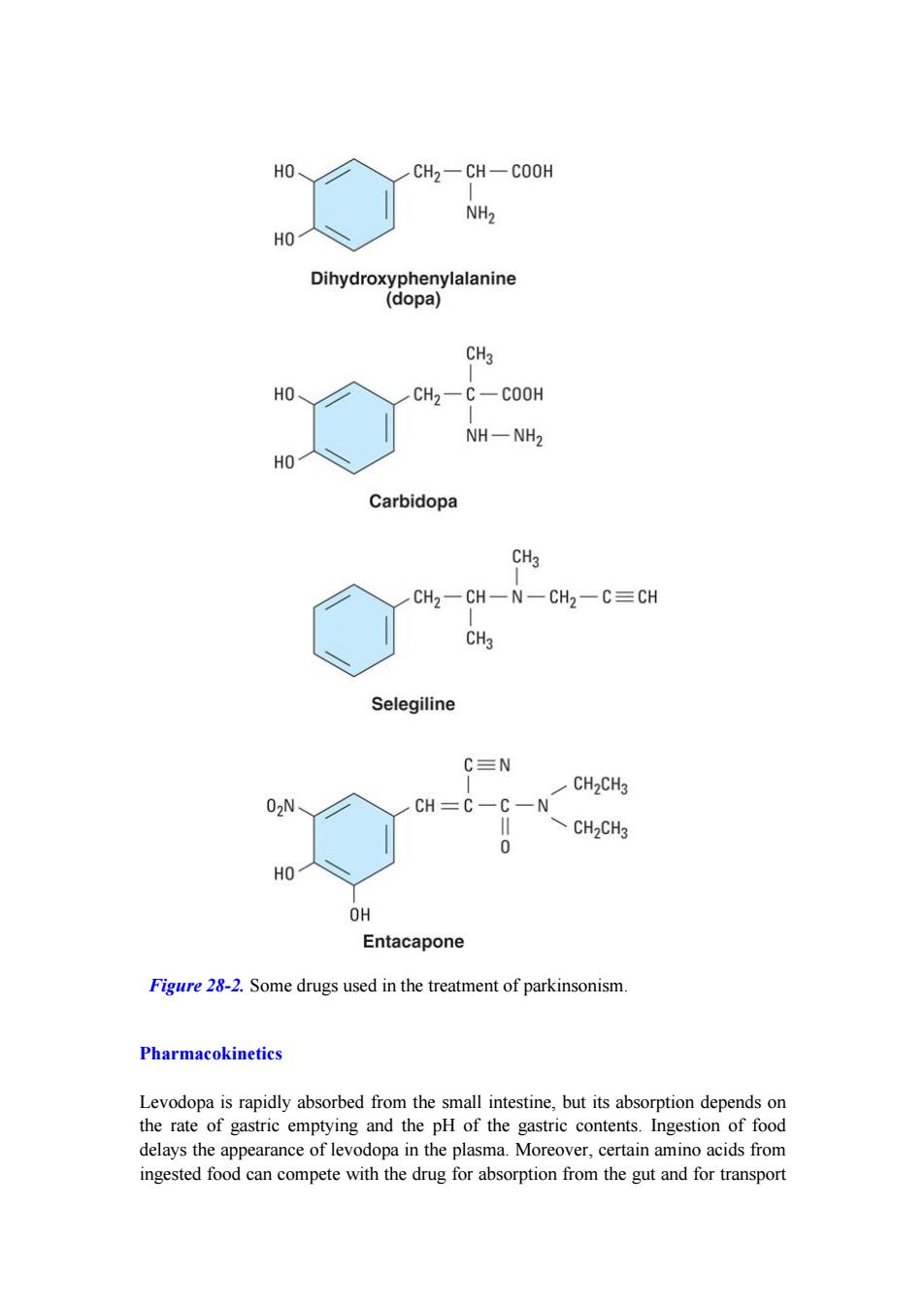
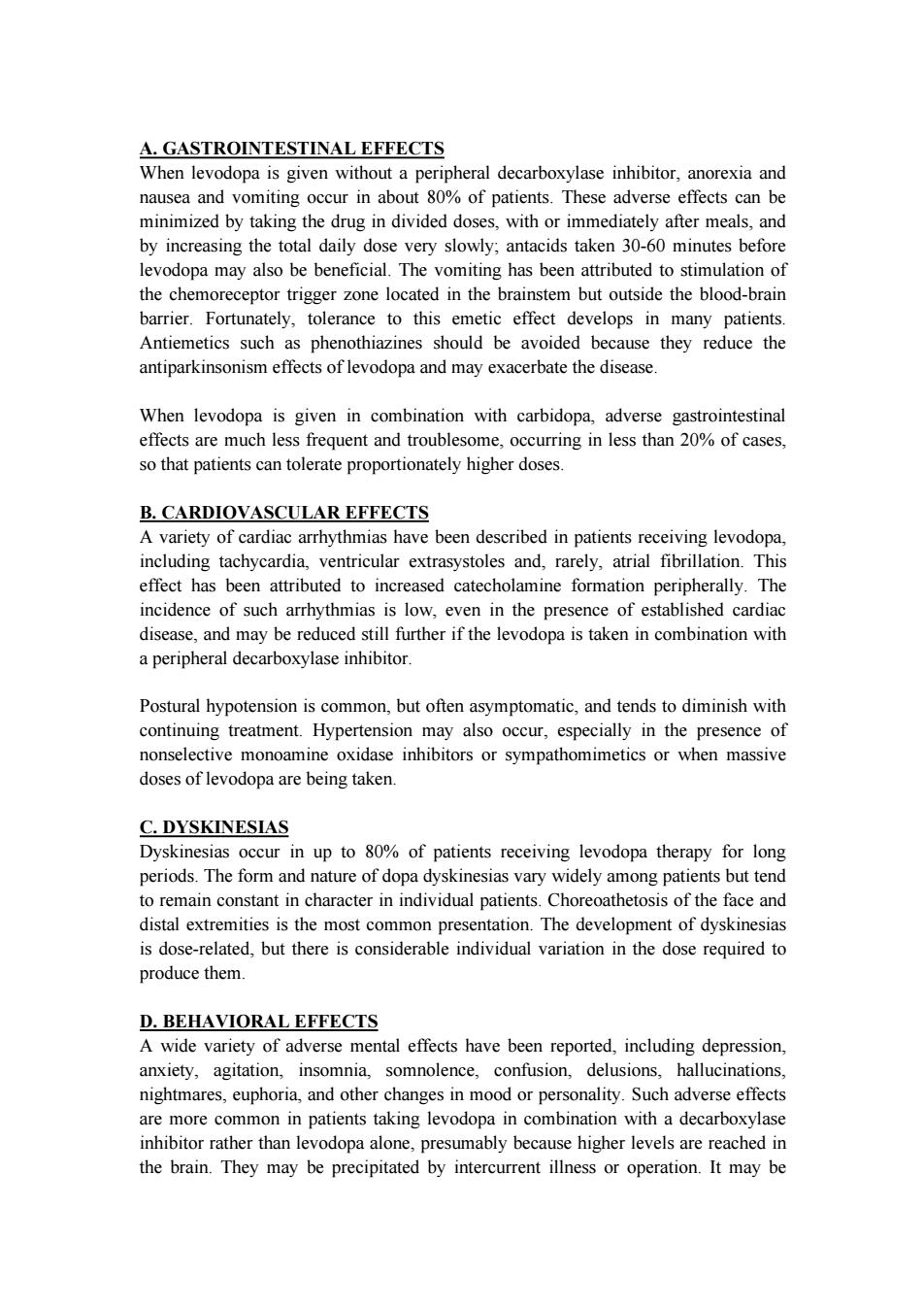
from the blood to the brain.Plasma concentrations usually peak between 1 and 2 hours after an oral dose,and the plasma half-life is usually between 1 and 3 hours, although it varies considerably among individuals.About two thirds of the dose appears in the urine as metabolites within 8 hours of an oral dose,the main metabolic products being 3-methoxy-4-hydroxyphenyl acetic acid (homovanillic acid,HVA) and dihydroxyphenylacetic acid (DOPAC).Unfortunately,only about 1-3%of administered levodopa actually enters the brain unaltered;the remainder is metabolized extra-cerebrally,predominantly by decarboxylation to dopamine,which does not penetrate the blood-brain barrier.This means that levodopa must be given in large amounts when it is used alone.However,when it is given in combination with a dopa decarboxylase inhibitor that does not penetrate the blood-brain barrier,the peripheral metabolism of levodopa is reduced,plasma levels of levodopa are higher, plasma half-life is longer,and more dopa is available for entry into the brain(Figure 28-3).Indeed,concomitant administration of a peripheral dopa decarboxylase inhibitor such as carbidopa may reduce the daily requirements of levodopa by approximately 75%. Levodopa alone 100% 30% 1-3% Brain Blood Levodopa dose Gut 70% 27-29% Metabolism Peripheral in the tissues GI tract (toxicity) Levodopa with carbidopa 100% 60% 10% Levodopa Gut Blood Brain dase 409 50% Metabolism Peripheral in the tissues Gl tract (toxicity) Figure 28-3.Fate of orally administered levodopa and the effect of carbidopa, estimated from animal data.The width of each pathway indicates the absolute amount of the drug at each site,whereas the percentages shown denote the relative proportion
from the blood to the brain. Plasma concentrations usually peak between 1 and 2 hours after an oral dose, and the plasma half-life is usually between 1 and 3 hours, although it varies considerably among individuals. About two thirds of the dose appears in the urine as metabolites within 8 hours of an oral dose, the main metabolic products being 3-methoxy-4-hydroxyphenyl acetic acid (homovanillic acid, HVA) and dihydroxyphenylacetic acid (DOPAC). Unfortunately, only about 1-3% of administered levodopa actually enters the brain unaltered; the remainder is metabolized extra-cerebrally, predominantly by decarboxylation to dopamine, which does not penetrate the blood-brain barrier. This means that levodopa must be given in large amounts when it is used alone. However, when it is given in combination with a dopa decarboxylase inhibitor that does not penetrate the blood-brain barrier, the peripheral metabolism of levodopa is reduced, plasma levels of levodopa are higher, plasma half-life is longer, and more dopa is available for entry into the brain (Figure 28-3). Indeed, concomitant administration of a peripheral dopa decarboxylase inhibitor such as carbidopa may reduce the daily requirements of levodopa by approximately 75%. Figure 28-3. Fate of orally administered levodopa and the effect of carbidopa, estimated from animal data. The width of each pathway indicates the absolute amount of the drug at each site, whereas the percentages shown denote the relative proportion

of the administered dose.The benefits of coadministration of carbidopa include reduction of the amount of levodopa diverted to peripheral tissues and an increase in the fraction of the dose that reaches the brain.(GI,gastrointestinal.)(Data from Nutt JG,Fellman JH:Pharmacokinetics of levodopa.Clin Neuropharmacol 1984;7:35.) Clinical Use The best results of levodopa treatment are obtained in the first few years of treatment. This is sometimes because the daily dose of levodopa must be reduced over time to avoid side effects at doses that were well tolerated at the outset.Some patients also become less responsive to levodopa,so that previously effective doses eventually fail to produce any therapeutic benefit.Responsiveness to levodopa may ultimately be lost completely,perhaps because of the disappearance of dopaminergic nigrostriatal nerve terminals or some pathologic process directly involving the striatal dopamine receptors.For such reasons,the benefits of levodopa treatment often begin to diminish after about 3 or 4 years of therapy regardless of the initial therapeutic response. Although levodopa therapy does not stop the progression of parkinsonism,its early initiation lowers the mortality rate.However,long-term therapy may lead to a number of problems in management such as the on-off phenomenon discussed below.The most appropriate time to introduce levodopa therapy must therefore be determined individually. When levodopa is used,it is generally given in combination with carbidopa(Figure 28-2),a peripheral dopa decarboxylase inhibitor,which reduces peripheral conversion to dopamine.Sinemet treatment is started with a small dose,eg,Sinemet-25/100 (carbidopa 25 mg,levodopa 100 mg)three times daily,and gradually increased.It should be taken 30-60 minutes before meals.Most patients ultimately require Sinemet-25/250(carbidopa 25 mg,levodopa 250 mg)three or four times daily.It is generally preferable to keep treatment with this agent at a low level (eg, Sinemet-25/100 three times daily)and to increase dopaminergic therapy by the addition of a dopamine agonist,if necessary,to reduce the risk of development of response fluctuations.A controlled-release formulation of Sinemet is available and may be helpful in patients with established response fluctuations or as a means of reducing dosing frequency.A commercially available combination (Stalevo)of levodopa,carbidopa,and a catechol-O-methyltransferase (COMT)inhibitor (entacapone)is discussed in a later section. Levodopa can ameliorate all of the clinical features of parkinsonism,but it is particularly effective in relieving bradykinesia and any disabilities resulting from it. When it is first introduced,about one third of patients respond very well and one third less well.Most of the remainder either are unable to tolerate the medication or simply do not respond at all. Adverse Effects
of the administered dose. The benefits of coadministration of carbidopa include reduction of the amount of levodopa diverted to peripheral tissues and an increase in the fraction of the dose that reaches the brain. (GI, gastrointestinal.) (Data from Nutt JG, Fellman JH: Pharmacokinetics of levodopa. Clin Neuropharmacol 1984;7:35.) Clinical Use The best results of levodopa treatment are obtained in the first few years of treatment. This is sometimes because the daily dose of levodopa must be reduced over time to avoid side effects at doses that were well tolerated at the outset. Some patients also become less responsive to levodopa, so that previously effective doses eventually fail to produce any therapeutic benefit. Responsiveness to levodopa may ultimately be lost completely, perhaps because of the disappearance of dopaminergic nigrostriatal nerve terminals or some pathologic process directly involving the striatal dopamine receptors. For such reasons, the benefits of levodopa treatment often begin to diminish after about 3 or 4 years of therapy regardless of the initial therapeutic response. Although levodopa therapy does not stop the progression of parkinsonism, its early initiation lowers the mortality rate. However, long-term therapy may lead to a number of problems in management such as the on-off phenomenon discussed below. The most appropriate time to introduce levodopa therapy must therefore be determined individually. When levodopa is used, it is generally given in combination with carbidopa (Figure 28-2), a peripheral dopa decarboxylase inhibitor, which reduces peripheral conversion to dopamine. Sinemet treatment is started with a small dose, eg, Sinemet-25/100 (carbidopa 25 mg, levodopa 100 mg) three times daily, and gradually increased. It should be taken 30-60 minutes before meals. Most patients ultimately require Sinemet-25/250 (carbidopa 25 mg, levodopa 250 mg) three or four times daily. It is generally preferable to keep treatment with this agent at a low level (eg, Sinemet-25/100 three times daily) and to increase dopaminergic therapy by the addition of a dopamine agonist, if necessary, to reduce the risk of development of response fluctuations. A controlled-release formulation of Sinemet is available and may be helpful in patients with established response fluctuations or as a means of reducing dosing frequency. A commercially available combination (Stalevo) of levodopa, carbidopa, and a catechol-O-methyltransferase (COMT) inhibitor (entacapone) is discussed in a later section. Levodopa can ameliorate all of the clinical features of parkinsonism, but it is particularly effective in relieving bradykinesia and any disabilities resulting from it. When it is first introduced, about one third of patients respond very well and one third less well. Most of the remainder either are unable to tolerate the medication or simply do not respond at all. Adverse Effects
A.GASTROINTESTINAL EFFECTS When levodopa is given without a peripheral decarboxylase inhibitor,anorexia and nausea and vomiting occur in about 80%of patients.These adverse effects can be minimized by taking the drug in divided doses,with or immediately after meals,and by increasing the total daily dose very slowly;antacids taken 30-60 minutes before levodopa may also be beneficial.The vomiting has been attributed to stimulation of the chemoreceptor trigger zone located in the brainstem but outside the blood-brain barrier.Fortunately,tolerance to this emetic effect develops in many patients. Antiemetics such as phenothiazines should be avoided because they reduce the antiparkinsonism effects of levodopa and may exacerbate the disease. When levodopa is given in combination with carbidopa,adverse gastrointestinal effects are much less frequent and troublesome,occurring in less than 20%of cases, so that patients can tolerate proportionately higher doses. B.CARDIOVASCULAR EFFECTS A variety of cardiac arrhythmias have been described in patients receiving levodopa, including tachycardia,ventricular extrasystoles and,rarely,atrial fibrillation.This effect has been attributed to increased catecholamine formation peripherally.The incidence of such arrhythmias is low,even in the presence of established cardiac disease,and may be reduced still further if the levodopa is taken in combination with a peripheral decarboxylase inhibitor. Postural hypotension is common,but often asymptomatic,and tends to diminish with continuing treatment.Hypertension may also occur,especially in the presence of nonselective monoamine oxidase inhibitors or sympathomimetics or when massive doses of levodopa are being taken. C.DYSKINESIAS Dyskinesias occur in up to 80%of patients receiving levodopa therapy for long periods.The form and nature of dopa dyskinesias vary widely among patients but tend to remain constant in character in individual patients.Choreoathetosis of the face and distal extremities is the most common presentation.The development of dyskinesias is dose-related.but there is considerable individual variation in the dose required to produce them. D.BEHAVIORAL EFFECTS A wide variety of adverse mental effects have been reported,including depression, anxiety,agitation,insomnia,somnolence,confusion,delusions,hallucinations, nightmares,euphoria,and other changes in mood or personality.Such adverse effects are more common in patients taking levodopa in combination with a decarboxylase inhibitor rather than levodopa alone,presumably because higher levels are reached in the brain.They may be precipitated by intercurrent illness or operation.It may be
A. GASTROINTESTINAL EFFECTS When levodopa is given without a peripheral decarboxylase inhibitor, anorexia and nausea and vomiting occur in about 80% of patients. These adverse effects can be minimized by taking the drug in divided doses, with or immediately after meals, and by increasing the total daily dose very slowly; antacids taken 30-60 minutes before levodopa may also be beneficial. The vomiting has been attributed to stimulation of the chemoreceptor trigger zone located in the brainstem but outside the blood-brain barrier. Fortunately, tolerance to this emetic effect develops in many patients. Antiemetics such as phenothiazines should be avoided because they reduce the antiparkinsonism effects of levodopa and may exacerbate the disease. When levodopa is given in combination with carbidopa, adverse gastrointestinal effects are much less frequent and troublesome, occurring in less than 20% of cases, so that patients can tolerate proportionately higher doses. B. CARDIOVASCULAR EFFECTS A variety of cardiac arrhythmias have been described in patients receiving levodopa, including tachycardia, ventricular extrasystoles and, rarely, atrial fibrillation. This effect has been attributed to increased catecholamine formation peripherally. The incidence of such arrhythmias is low, even in the presence of established cardiac disease, and may be reduced still further if the levodopa is taken in combination with a peripheral decarboxylase inhibitor. Postural hypotension is common, but often asymptomatic, and tends to diminish with continuing treatment. Hypertension may also occur, especially in the presence of nonselective monoamine oxidase inhibitors or sympathomimetics or when massive doses of levodopa are being taken. C. DYSKINESIAS Dyskinesias occur in up to 80% of patients receiving levodopa therapy for long periods. The form and nature of dopa dyskinesias vary widely among patients but tend to remain constant in character in individual patients. Choreoathetosis of the face and distal extremities is the most common presentation. The development of dyskinesias is dose-related, but there is considerable individual variation in the dose required to produce them. D. BEHAVIORAL EFFECTS A wide variety of adverse mental effects have been reported, including depression, anxiety, agitation, insomnia, somnolence, confusion, delusions, hallucinations, nightmares, euphoria, and other changes in mood or personality. Such adverse effects are more common in patients taking levodopa in combination with a decarboxylase inhibitor rather than levodopa alone, presumably because higher levels are reached in the brain. They may be precipitated by intercurrent illness or operation. It may be
necessary to reduce or withdraw the medication.Several atypical antipsychotic agents (clozapine,olanzapine,quetiapine,and risperidone;see Chapter 29)are now available and may be particularly helpful in counteracting the behavioral complications of levodopa. E.FLUCTUATIONS IN RESPONSE Certain fluctuations in clinical response to levodopa occur with increasing frequency as treatment continues.In some patients,these fluctuations relate to the timing of levodopa intake,and they are then referred to as wearing-off reactions or end-of-dose akinesia.In other instances,fluctuations in clinical state are unrelated to the timing of doses (on-off phenomenon).In the on-off phenomenon,off-periods of marked akinesia alternate over the course of a few hours with on-periods of improved mobility but often marked dyskinesia.The phenomenon is most likely to occur in patients who responded well to treatment initially.The exact mechanism is unknown. For patients with severe off-periods who are unresponsive to other measures, subcutaneously injected apomorphine may provide temporary benefit. F.MISCELLANEOUS ADVERSE EFFECTS Mydriasis may occur and may precipitate an attack of acute glaucoma in some patients.Other reported but rare adverse effects include various blood dyscrasias;a positive Coombs test with evidence of hemolysis;hot flushes;aggravation or precipitation of gout;abnormalities of smell or taste;brownish discoloration of saliva, urine,or vaginal secretions;priapism;and mildusually transientelevations of blood urea nitrogen and of serum transaminases,alkaline phosphatase,and bilirubin. Drug Holidays A drug holiday (discontinuance of the drug for 3-21 days)may temporarily improve responsiveness to levodopa and alleviate some of its adverse effects but is usually of little help in the management of the on-off phenomenon.Furthermore,a drug holiday carries the risks of aspiration pneumonia,venous thrombosis,pulmonary embolism, and depression resulting from the immobility accompanying severe parkinsonism.For these reasons and because of the temporary nature of any benefit,drug holidays are no longer recommended. Drug Interactions Pharmacologic doses of pyridoxine (vitamin B6)enhance the extracerebral metabolism of levodopa and may therefore prevent its therapeutic effect unless a peripheral decarboxylase inhibitor is also taken.Levodopa should not be given to patients taking monoamine oxidase A inhibitors or within 2 weeks of their discontinuance,because such a combination can lead to hypertensive crises. Contraindications
necessary to reduce or withdraw the medication. Several atypical antipsychotic agents (clozapine, olanzapine, quetiapine, and risperidone; see Chapter 29) are now available and may be particularly helpful in counteracting the behavioral complications of levodopa. E. FLUCTUATIONS IN RESPONSE Certain fluctuations in clinical response to levodopa occur with increasing frequency as treatment continues. In some patients, these fluctuations relate to the timing of levodopa intake, and they are then referred to as wearing-off reactions or end-of-dose akinesia. In other instances, fluctuations in clinical state are unrelated to the timing of doses (on-off phenomenon). In the on-off phenomenon, off-periods of marked akinesia alternate over the course of a few hours with on-periods of improved mobility but often marked dyskinesia. The phenomenon is most likely to occur in patients who responded well to treatment initially. The exact mechanism is unknown. For patients with severe off-periods who are unresponsive to other measures, subcutaneously injected apomorphine may provide temporary benefit. F. MISCELLANEOUS ADVERSE EFFECTS Mydriasis may occur and may precipitate an attack of acute glaucoma in some patients. Other reported but rare adverse effects include various blood dyscrasias; a positive Coombs test with evidence of hemolysis; hot flushes; aggravation or precipitation of gout; abnormalities of smell or taste; brownish discoloration of saliva, urine, or vaginal secretions; priapism; and mild¾usually transient¾elevations of blood urea nitrogen and of serum transaminases, alkaline phosphatase, and bilirubin. Drug Holidays A drug holiday (discontinuance of the drug for 3-21 days) may temporarily improve responsiveness to levodopa and alleviate some of its adverse effects but is usually of little help in the management of the on-off phenomenon. Furthermore, a drug holiday carries the risks of aspiration pneumonia, venous thrombosis, pulmonary embolism, and depression resulting from the immobility accompanying severe parkinsonism. For these reasons and because of the temporary nature of any benefit, drug holidays are no longer recommended. Drug Interactions Pharmacologic doses of pyridoxine (vitamin B6) enhance the extracerebral metabolism of levodopa and may therefore prevent its therapeutic effect unless a peripheral decarboxylase inhibitor is also taken. Levodopa should not be given to patients taking monoamine oxidase A inhibitors or within 2 weeks of their discontinuance, because such a combination can lead to hypertensive crises. Contraindications
Levodopa should not be given to psychotic patients because it may exacerbate the mental disturbance.It is also contraindicated in patients with angle-closure glaucoma, but those with chronic open-angle glaucoma may be given levodopa if intraocular pressure is well controlled and can be monitored.It is best given combined with carbidopa to patients with cardiac disease;even so,the risk of cardiac dysrhythmia is slight.Patients with active peptic ulcer must also be managed carefully,since gastrointestinal bleeding has occasionally occurred with levodopa.Because levodopa is a precursor of skin melanin and conceivably may activate malignant melanoma,its use should be avoided in patients with a history of melanoma or with suspicious undiagnosed skin lesions. DOPAMINE RECEPTOR AGONISTS Introduction Drugs acting directly on dopamine receptors may have a beneficial effect in addition to that of levodopa.Unlike levodopa,they do not require enzymatic conversion to an active metabolite,have no potentially toxic metabolites,and do not compete with other substances for active transport into the blood and across the blood-brain barrier. Moreover,drugs selectively affecting certain (but not all)dopamine receptors may have more limited adverse effects than levodopa.A number of dopamine agonists have antiparkinsonism activity.The older dopamine agonists (bromocriptine and pergolide)are ergot (ergoline)derivatives (see Chapter 16),and their side effects are of more concern than those of the newer agents(pramipexole and ropinirole).There is no evidence that one agonist is superior to another;individual patients,however,may respond to one but not another of these agents.Apomorphine is a potent dopamine agonist but is discussed separately in a later section in this chapter because it is used primarily as a rescue drug for patients with disabling response fluctuations to levodopa. Dopamine agonists have an important role as first-line therapy for Parkinson's disease, and their use is associated with a lower incidence of the response fluctuations and dyskinesias that occur with long-term levodopa therapy.In consequence, dopaminergic therapy may best be initiated with a dopamine agonist.Alternatively,a low dose of carbidopa plus levodopa (eg,Sinemet-25/100 three times daily)is introduced and a dopamine agonist is then added.In either case,the dose of the dopamine agonist is built up gradually depending on response and tolerance. Dopamine agonists may also be given to patients with parkinsonism who are taking levodopa and who have end-of-dose akinesia or on-off phenomenon or are becoming resistant to treatment with levodopa.In such circumstances,it is generally necessary to lower the dose of levodopa to prevent intolerable adverse effects.The response to a dopamine agonist is generally disappointing in patients who have never responded to levodopa
Levodopa should not be given to psychotic patients because it may exacerbate the mental disturbance. It is also contraindicated in patients with angle-closure glaucoma, but those with chronic open-angle glaucoma may be given levodopa if intraocular pressure is well controlled and can be monitored. It is best given combined with carbidopa to patients with cardiac disease; even so, the risk of cardiac dysrhythmia is slight. Patients with active peptic ulcer must also be managed carefully, since gastrointestinal bleeding has occasionally occurred with levodopa. Because levodopa is a precursor of skin melanin and conceivably may activate malignant melanoma, its use should be avoided in patients with a history of melanoma or with suspicious undiagnosed skin lesions. DOPAMINE RECEPTOR AGONISTS Introduction Drugs acting directly on dopamine receptors may have a beneficial effect in addition to that of levodopa. Unlike levodopa, they do not require enzymatic conversion to an active metabolite, have no potentially toxic metabolites, and do not compete with other substances for active transport into the blood and across the blood-brain barrier. Moreover, drugs selectively affecting certain (but not all) dopamine receptors may have more limited adverse effects than levodopa. A number of dopamine agonists have antiparkinsonism activity. The older dopamine agonists (bromocriptine and pergolide) are ergot (ergoline) derivatives (see Chapter 16), and their side effects are of more concern than those of the newer agents (pramipexole and ropinirole). There is no evidence that one agonist is superior to another; individual patients, however, may respond to one but not another of these agents. Apomorphine is a potent dopamine agonist but is discussed separately in a later section in this chapter because it is used primarily as a rescue drug for patients with disabling response fluctuations to levodopa. Dopamine agonists have an important role as first-line therapy for Parkinson's disease, and their use is associated with a lower incidence of the response fluctuations and dyskinesias that occur with long-term levodopa therapy. In consequence, dopaminergic therapy may best be initiated with a dopamine agonist. Alternatively, a low dose of carbidopa plus levodopa (eg, Sinemet-25/100 three times daily) is introduced and a dopamine agonist is then added. In either case, the dose of the dopamine agonist is built up gradually depending on response and tolerance. Dopamine agonists may also be given to patients with parkinsonism who are taking levodopa and who have end-of-dose akinesia or on-off phenomenon or are becoming resistant to treatment with levodopa. In such circumstances, it is generally necessary to lower the dose of levodopa to prevent intolerable adverse effects. The response to a dopamine agonist is generally disappointing in patients who have never responded to levodopa