English Reading Materials Chapter 27:Histamine INTRODUCTION Histamine and serotonin(5-hydroxytryptamine)are biologically active amines that function as neurotransmitters and are found in non-neural tissues,have complex physiologic and pathologic effects through multiple receptor subtypes,and are often released locally.Together with endogenous peptides,prostaglandins and leukotrienes, and cytokines,they are sometimes called autacoids (Greek,"self-remedy")or local hormones in recognition of these properties. Because of their broad and largely undesirable effects,neither histamine nor serotonin has any clinical application in the treatment of disease.However,compounds that selectively activate certain receptor subtypes or selectively antagonize the actions of these amines are of considerable clinical usefulness.This chapter therefore emphasizes the basic pharmacology of the agonist amines and the clinical pharmacology of the more selective agonist and antagonist drugs.The ergot alkaloids, compounds with partial agonist activity at serotonin and several other receptors,are discussed at the end of the chapter. I.HISTAMINE INTRODUCTION Histamine was synthesized in 1907 and later isolated from mammalian tissues.Early hypotheses concerning the possible physiologic roles of tissue histamine were based on similarities between the effects of intravenously administered histamine and the symptoms of anaphylactic shock and tissue injury.Marked species variation is observed,but in humans histamine is an important mediator of immediate allergic and inflammatory reactions,although it plays only a modest role in anaphylaxis. Histamine plays an important role in gastric acid secretion and functions as a neurotransmitter and neuromodulator.Newer evidence indicates that histamine also plays a role in chemotaxis of white blood cells. BASIC PHARMACOLOGY OF HISTAMINE Chemistry Pharmacokinetics Histamine occurs in plants as well as in animal tissues and is a component of some venoms and stinging secretions
English Reading Materials Chapter 27: Histamine INTRODUCTION Histamine and serotonin (5-hydroxytryptamine) are biologically active amines that function as neurotransmitters and are found in non-neural tissues, have complex physiologic and pathologic effects through multiple receptor subtypes, and are often released locally. Together with endogenous peptides, prostaglandins and leukotrienes, and cytokines, they are sometimes called autacoids (Greek, "self-remedy") or local hormones in recognition of these properties. Because of their broad and largely undesirable effects, neither histamine nor serotonin has any clinical application in the treatment of disease. However, compounds that selectively activate certain receptor subtypes or selectively antagonize the actions of these amines are of considerable clinical usefulness. This chapter therefore emphasizes the basic pharmacology of the agonist amines and the clinical pharmacology of the more selective agonist and antagonist drugs. The ergot alkaloids, compounds with partial agonist activity at serotonin and several other receptors, are discussed at the end of the chapter. I. HISTAMINE INTRODUCTION Histamine was synthesized in 1907 and later isolated from mammalian tissues. Early hypotheses concerning the possible physiologic roles of tissue histamine were based on similarities between the effects of intravenously administered histamine and the symptoms of anaphylactic shock and tissue injury. Marked species variation is observed, but in humans histamine is an important mediator of immediate allergic and inflammatory reactions, although it plays only a modest role in anaphylaxis. Histamine plays an important role in gastric acid secretion and functions as a neurotransmitter and neuromodulator. Newer evidence indicates that histamine also plays a role in chemotaxis of white blood cells. BASIC PHARMACOLOGY OF HISTAMINE Chemistry Pharmacokinetics Histamine occurs in plants as well as in animal tissues and is a component of some venoms and stinging secretions
Histamine is formed by decarboxylation of the amino acid /-histidine,a reaction catalyzed in mammalian tissues by the enzyme histidine decarboxylase.Once formed, histamine is either stored or rapidly inactivated.Very little histamine is excreted unchanged.The major metabolic pathways involve conversion to N-methylhistamine, methylimidazoleacetic acid,and imidazoleacetic acid (IAA).Certain neoplasms (systemic mastocytosis,urticaria pigmentosa,gastric carcinoid,and occasionally myelogenous leukemia)are associated with increased numbers of mast cells or basophils and with increased excretion of histamine and its metabolites. Most tissue histamine is sequestered and bound in granules(vesicles)in mast cells or basophils;the histamine content of many tissues is directly related to their mast cell content.The bound form of histamine is biologically inactive,but many stimuli,as noted below,can trigger the release of mast cell histamine,allowing the free amine to exert its actions on surrounding tissues.Mast cells are especially rich at sites of potential tissue injury nose,mouth,and feet;internal body surfaces;and blood vessels,particularly at pressure points and bifurcations. Non-mast cell histamine is found in several tissues,including the brain,where it functions as a neurotransmitter.Endogenous neurotransmitter histamine may play a role in many brain functions such as neuroendocrine control,cardiovascular regulation,thermal and body weight regulation,and arousal. A second important nonneuronal site of histamine storage and release is the enterochromaffin-like (ECL)cells of the fundus of the stomach.ECL cells release histamine,one of the primary gastric acid secretagogues,to activate the acid-producing parietal cells of the mucosa. Storage Release of Histamine The stores of histamine in mast cells can be released through several mechanisms A.IMMUNOLOGIC RELEASE Immunologic processes account for the most important pathophysiologic mechanism of mast cell and basophil histamine release.These cells,if sensitized by IgE antibodies attached to their surface membranes,degranulate "explosively"when exposed to the appropriate antigen(see Figure 1,effector phase).This type of release also requires energy and calcium.Degranulation leads to the simultaneous release of histamine,adenosine triphosphate (ATP),and other mediators that are stored together in the granules.Histamine released by this mechanism is a mediator in immediate (type I)allergic reactions.Substances released during IgG-or IgM-mediated immune
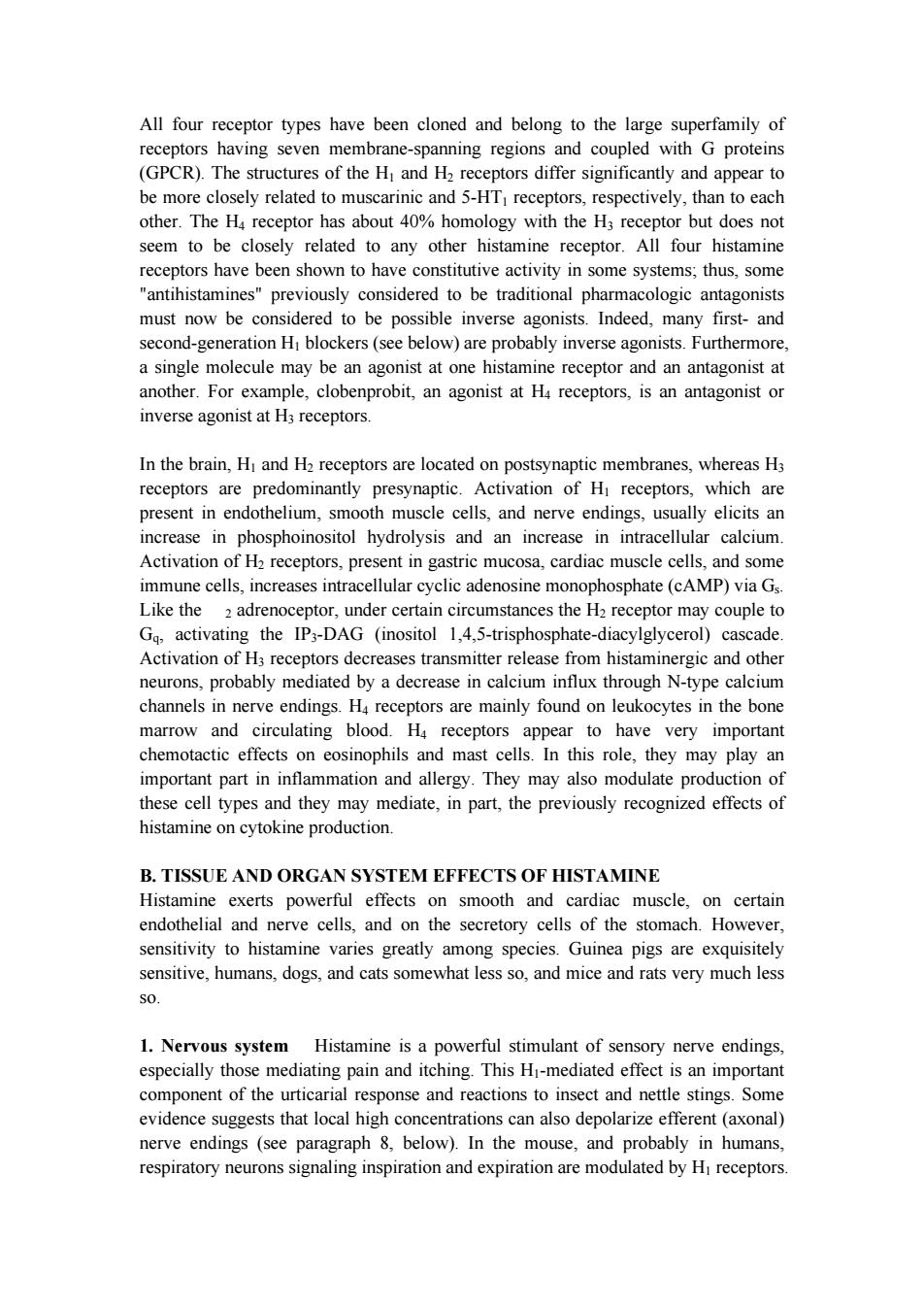
Histamine is formed by decarboxylation of the amino acid l-histidine, a reaction catalyzed in mammalian tissues by the enzyme histidine decarboxylase. Once formed, histamine is either stored or rapidly inactivated. Very little histamine is excreted unchanged. The major metabolic pathways involve conversion to N-methylhistamine, methylimidazoleacetic acid, and imidazoleacetic acid (IAA). Certain neoplasms (systemic mastocytosis, urticaria pigmentosa, gastric carcinoid, and occasionally myelogenous leukemia) are associated with increased numbers of mast cells or basophils and with increased excretion of histamine and its metabolites. Most tissue histamine is sequestered and bound in granules (vesicles) in mast cells or basophils; the histamine content of many tissues is directly related to their mast cell content. The bound form of histamine is biologically inactive, but many stimuli, as noted below, can trigger the release of mast cell histamine, allowing the free amine to exert its actions on surrounding tissues. Mast cells are especially rich at sites of potential tissue injury nose, mouth, and feet; internal body surfaces; and blood vessels, particularly at pressure points and bifurcations. Non-mast cell histamine is found in several tissues, including the brain, where it functions as a neurotransmitter. Endogenous neurotransmitter histamine may play a role in many brain functions such as neuroendocrine control, cardiovascular regulation, thermal and body weight regulation, and arousal. A second important nonneuronal site of histamine storage and release is the enterochromaffin-like (ECL) cells of the fundus of the stomach. ECL cells release histamine, one of the primary gastric acid secretagogues, to activate the acid-producing parietal cells of the mucosa. Storage Release of Histamine The stores of histamine in mast cells can be released through several mechanisms. A. IMMUNOLOGIC RELEASE Immunologic processes account for the most important pathophysiologic mechanism of mast cell and basophil histamine release. These cells, if sensitized by IgE antibodies attached to their surface membranes, degranulate "explosively" when exposed to the appropriate antigen (see Figure 1, effector phase). This type of release also requires energy and calcium. Degranulation leads to the simultaneous release of histamine, adenosine triphosphate (ATP), and other mediators that are stored together in the granules. Histamine released by this mechanism is a mediator in immediate (type I) allergic reactions. Substances released during IgG- or IgM-mediated immune
reactions that activate the complement cascade also release histamine from mast cells and basophils. By a negative feedback control mechanism mediated by H2 receptors,histamine appears to modulate its own release and that of other mediators from sensitized mast cells in some tissues.In humans,mast cells in skin and basophils show this negative feedback mechanism;lung mast cells do not.Thus,histamine may act to limit the intensity of the allergic reaction in the skin and blood. Endogenous histamine has a modulating role in a variety of inflammatory and immune responses.Upon injury to a tissue,released histamine causes local vasodilation and leakage of plasma containing mediators of acute inflammation (complement,C-reactive protein),and antibodies.Histamine has an active chemotactic attraction for inflammatory cells (neutrophils,eosinophils,basophils, monocytes,and lymphocytes).Histamine inhibits the release of lysosome contents and several T-and B-lymphocyte functions.Most of these actions are mediated by H2 or H4 receptors.Release of peptides from nerves in response to inflammation is also probably modulated by histamine,in this case acting through presynaptic H3 receptors. B.CHEMICAL AND MECHANICAL RELEASE Certain amines,including drugs such as morphine and tubocurarine,can displace histamine from the heparin-protein complex within cells.This type of release does not require energy and is not associated with mast cell injury or degranulation.Loss of granules from the mast cell also releases histamine,since sodium ions in the extracellular fluid rapidly displace the amine from the complex.Chemical and mechanical mast cell injury causes degranulation and histamine release.Compound 48/80,an experimental drug,selectively releases histamine from tissue mast cells by an exocytotic degranulation process requiring energy and calcium
reactions that activate the complement cascade also release histamine from mast cells and basophils. By a negative feedback control mechanism mediated by H2 receptors, histamine appears to modulate its own release and that of other mediators from sensitized mast cells in some tissues. In humans, mast cells in skin and basophils show this negative feedback mechanism; lung mast cells do not. Thus, histamine may act to limit the intensity of the allergic reaction in the skin and blood. Endogenous histamine has a modulating role in a variety of inflammatory and immune responses. Upon injury to a tissue, released histamine causes local vasodilation and leakage of plasma containing mediators of acute inflammation (complement, C-reactive protein), and antibodies. Histamine has an active chemotactic attraction for inflammatory cells (neutrophils, eosinophils, basophils, monocytes, and lymphocytes). Histamine inhibits the release of lysosome contents and several T- and B-lymphocyte functions. Most of these actions are mediated by H2 or H4 receptors. Release of peptides from nerves in response to inflammation is also probably modulated by histamine, in this case acting through presynaptic H3 receptors. B. CHEMICAL AND MECHANICAL RELEASE Certain amines, including drugs such as morphine and tubocurarine, can displace histamine from the heparin-protein complex within cells. This type of release does not require energy and is not associated with mast cell injury or degranulation. Loss of granules from the mast cell also releases histamine, since sodium ions in the extracellular fluid rapidly displace the amine from the complex. Chemical and mechanical mast cell injury causes degranulation and histamine release. Compound 48/80, an experimental drug, selectively releases histamine from tissue mast cells by an exocytotic degranulation process requiring energy and calcium
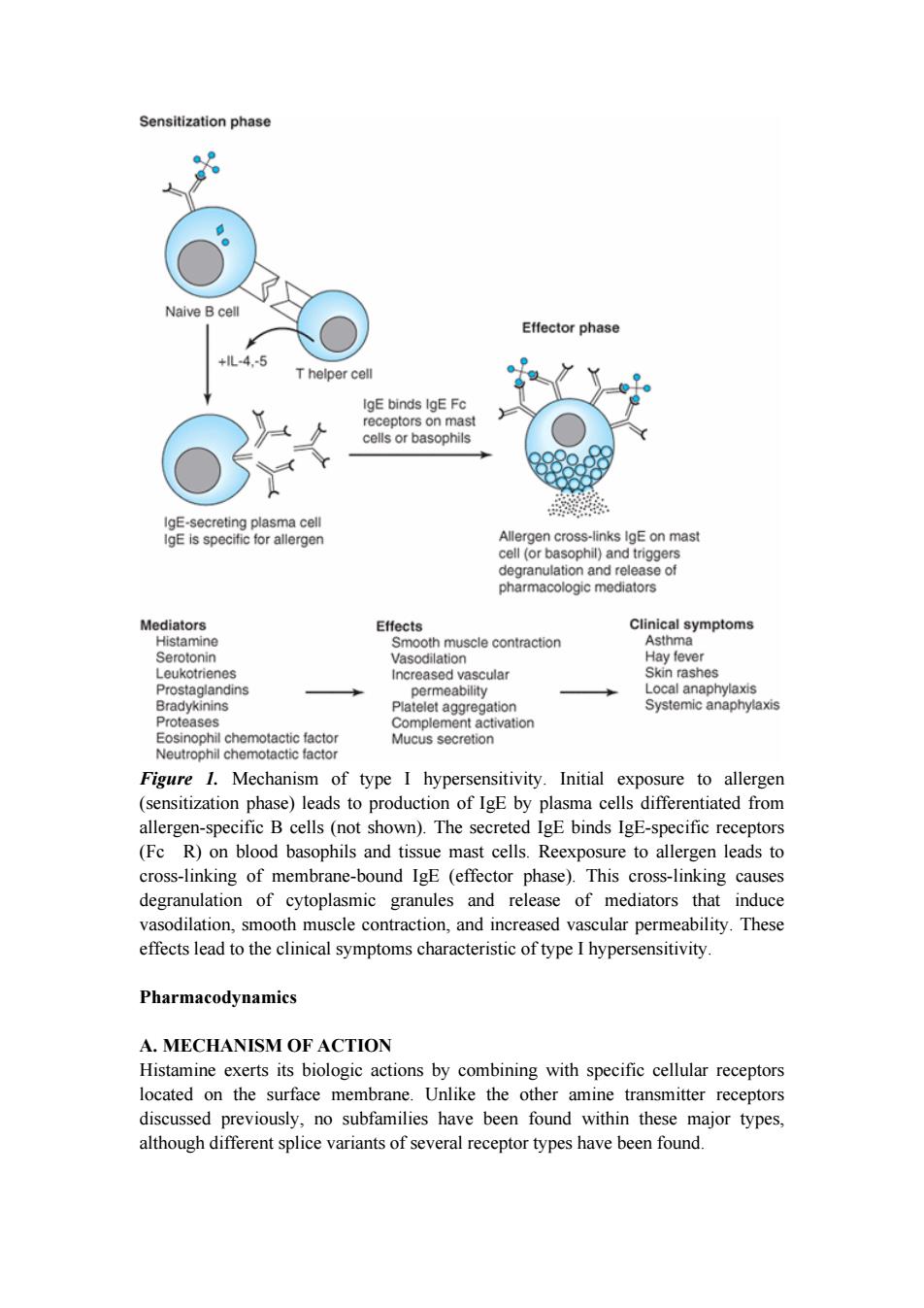
Sensitization phase Naive Bcell Effector phase +lL-4-5 T helper cell IgE binds IgE Fc receptors on mast cells or basophils IgE-secreting plasma cell IgE is specific for allergen Allergen cross-links IgE on mast cell (or basophil)and triggers degranulation and release of pharmacologic mediators Mediators Effects Clinical symptoms Histamine Smooth muscle contraction Asthma Serotonin Vasodilation Hay fever Leukotrienes Increased vascular Skin rashes Prostaglandins permeability Local anaphylaxis Bradykinins Platelet aggregation Systemic anaphylaxis Proteases Complement activation Eosinophil chemotactic factor Mucus secretion Neutrophil chemotactic factor Figure 1.Mechanism of type I hypersensitivity.Initial exposure to allergen (sensitization phase)leads to production of IgE by plasma cells differentiated from allergen-specific B cells(not shown).The secreted IgE binds IgE-specific receptors (Fc R)on blood basophils and tissue mast cells.Reexposure to allergen leads to cross-linking of membrane-bound IgE (effector phase).This cross-linking causes degranulation of cytoplasmic granules and release of mediators that induce vasodilation,smooth muscle contraction,and increased vascular permeability.These effects lead to the clinical symptoms characteristic of type I hypersensitivity Pharmacodynamics A.MECHANISM OF ACTION Histamine exerts its biologic actions by combining with specific cellular receptors located on the surface membrane.Unlike the other amine transmitter receptors discussed previously,no subfamilies have been found within these major types, although different splice variants of several receptor types have been found
Figure 1. Mechanism of type I hypersensitivity. Initial exposure to allergen (sensitization phase) leads to production of IgE by plasma cells differentiated from allergen-specific B cells (not shown). The secreted IgE binds IgE-specific receptors (Fc R) on blood basophils and tissue mast cells. Reexposure to allergen leads to cross-linking of membrane-bound IgE (effector phase). This cross-linking causes degranulation of cytoplasmic granules and release of mediators that induce vasodilation, smooth muscle contraction, and increased vascular permeability. These effects lead to the clinical symptoms characteristic of type I hypersensitivity. Pharmacodynamics A. MECHANISM OF ACTION Histamine exerts its biologic actions by combining with specific cellular receptors located on the surface membrane. Unlike the other amine transmitter receptors discussed previously, no subfamilies have been found within these major types, although different splice variants of several receptor types have been found
All four receptor types have been cloned and belong to the large superfamily of receptors having seven membrane-spanning regions and coupled with G proteins (GPCR).The structures of the H and H2 receptors differ significantly and appear to be more closely related to muscarinic and 5-HTI receptors,respectively,than to each other.The H4 receptor has about 40%homology with the H3 receptor but does not seem to be closely related to any other histamine receptor.All four histamine receptors have been shown to have constitutive activity in some systems;thus,some "antihistamines"previously considered to be traditional pharmacologic antagonists must now be considered to be possible inverse agonists.Indeed,many first-and second-generation HI blockers(see below)are probably inverse agonists.Furthermore, a single molecule may be an agonist at one histamine receptor and an antagonist at another.For example,clobenprobit,an agonist at H4 receptors,is an antagonist or inverse agonist at H3 receptors. In the brain,Hi and H2 receptors are located on postsynaptic membranes,whereas H3 receptors are predominantly presynaptic.Activation of Hi receptors,which are present in endothelium,smooth muscle cells,and nerve endings,usually elicits an increase in phosphoinositol hydrolysis and an increase in intracellular calcium. Activation of H2 receptors,present in gastric mucosa,cardiac muscle cells,and some immune cells,increases intracellular cyclic adenosine monophosphate(cAMP)via Gs. Like the 2 adrenoceptor,under certain circumstances the H2 receptor may couple to Gq,activating the IP3-DAG (inositol 1,4,5-trisphosphate-diacylglycerol)cascade. Activation of H3 receptors decreases transmitter release from histaminergic and other neurons,probably mediated by a decrease in calcium influx through N-type calcium channels in nerve endings.H4 receptors are mainly found on leukocytes in the bone marrow and circulating blood.H4 receptors appear to have very important chemotactic effects on eosinophils and mast cells.In this role,they may play an important part in inflammation and allergy.They may also modulate production of these cell types and they may mediate,in part,the previously recognized effects of histamine on cytokine production. B.TISSUE AND ORGAN SYSTEM EFFECTS OF HISTAMINE Histamine exerts powerful effects on smooth and cardiac muscle,on certain endothelial and nerve cells,and on the secretory cells of the stomach.However, sensitivity to histamine varies greatly among species.Guinea pigs are exquisitely sensitive,humans,dogs,and cats somewhat less so,and mice and rats very much less SO 1.Nervous system Histamine is a powerful stimulant of sensory nerve endings, especially those mediating pain and itching.This Hi-mediated effect is an important component of the urticarial response and reactions to insect and nettle stings.Some evidence suggests that local high concentrations can also depolarize efferent(axonal) nerve endings (see paragraph 8,below).In the mouse,and probably in humans, respiratory neurons signaling inspiration and expiration are modulated by Hi receptors
All four receptor types have been cloned and belong to the large superfamily of receptors having seven membrane-spanning regions and coupled with G proteins (GPCR). The structures of the H1 and H2 receptors differ significantly and appear to be more closely related to muscarinic and 5-HT1 receptors, respectively, than to each other. The H4 receptor has about 40% homology with the H3 receptor but does not seem to be closely related to any other histamine receptor. All four histamine receptors have been shown to have constitutive activity in some systems; thus, some "antihistamines" previously considered to be traditional pharmacologic antagonists must now be considered to be possible inverse agonists. Indeed, many first- and second-generation H1 blockers (see below) are probably inverse agonists. Furthermore, a single molecule may be an agonist at one histamine receptor and an antagonist at another. For example, clobenprobit, an agonist at H4 receptors, is an antagonist or inverse agonist at H3 receptors. In the brain, H1 and H2 receptors are located on postsynaptic membranes, whereas H3 receptors are predominantly presynaptic. Activation of H1 receptors, which are present in endothelium, smooth muscle cells, and nerve endings, usually elicits an increase in phosphoinositol hydrolysis and an increase in intracellular calcium. Activation of H2 receptors, present in gastric mucosa, cardiac muscle cells, and some immune cells, increases intracellular cyclic adenosine monophosphate (cAMP) via Gs. Like the 2 adrenoceptor, under certain circumstances the H2 receptor may couple to Gq, activating the IP3-DAG (inositol 1,4,5-trisphosphate-diacylglycerol) cascade. Activation of H3 receptors decreases transmitter release from histaminergic and other neurons, probably mediated by a decrease in calcium influx through N-type calcium channels in nerve endings. H4 receptors are mainly found on leukocytes in the bone marrow and circulating blood. H4 receptors appear to have very important chemotactic effects on eosinophils and mast cells. In this role, they may play an important part in inflammation and allergy. They may also modulate production of these cell types and they may mediate, in part, the previously recognized effects of histamine on cytokine production. B. TISSUE AND ORGAN SYSTEM EFFECTS OF HISTAMINE Histamine exerts powerful effects on smooth and cardiac muscle, on certain endothelial and nerve cells, and on the secretory cells of the stomach. However, sensitivity to histamine varies greatly among species. Guinea pigs are exquisitely sensitive, humans, dogs, and cats somewhat less so, and mice and rats very much less so. 1. Nervous system Histamine is a powerful stimulant of sensory nerve endings, especially those mediating pain and itching. This H1-mediated effect is an important component of the urticarial response and reactions to insect and nettle stings. Some evidence suggests that local high concentrations can also depolarize efferent (axonal) nerve endings (see paragraph 8, below). In the mouse, and probably in humans, respiratory neurons signaling inspiration and expiration are modulated by H1 receptors
Presynaptic H3 receptors play important roles in modulating transmitter release in the nervous system.H3 agonists reduce the release of acetylcholine,amine,and peptide transmitters in various areas of the brain and in peripheral nerves. 2.Cardiovascular system In humans,injection or infusion of histamine causes a decrease in systolic and diastolic blood pressure and an increase in heart rate.The blood pressure changes are caused by the direct vasodilator action of histamine on arterioles and precapillary sphincters;the increase in heart rate involves both stimulatory actions of histamine on the heart and a reflex tachycardia.Flushing,a sense of warmth,and headache may also occur during histamine administration, consistent with the vasodilation.Vasodilation elicited by small doses of histamine is caused by Hi-receptor activation and is mediated primarily by release of nitric oxide from the endothelium.The decrease in blood pressure is usually accompanied by a reflex tachycardia.Higher doses of histamine activate the H2-mediated cAMP process of vasodilation and direct cardiac stimulation.In humans,the cardiovascular effects of small doses of histamine can usually be antagonized by Hi-receptor antagonists alone. Histamine-induced edema results from the action of the amine on HI receptors in the vessels of the microcirculation,especially the postcapillary vessels.The effect is associated with the separation of the endothelial cells,which permits the transudation of fluid and molecules as large as small proteins into the perivascular tissue.This effect is responsible for the urticaria(hives)that signals the release of histamine in the skin.Studies of endothelial cells suggest that actin and myosin within these cells contract,resulting in separation of the endothelial cells and increased permeability. Direct cardiac effects of histamine include both increased contractility and increased pacemaker rate.These effects are mediated chiefly by H2 receptors.In human atrial muscle,histamine can also decrease contractility;this effect is mediated by H receptors.The physiologic significance of these cardiac actions is not clear.Some of the cardiovascular signs and symptoms of anaphylaxis are due to released histamine, though several other mediators are involved and appear to be more important than histamine in humans. 3.Bronchiolar smooth muscle In both humans and guinea pigs,histamine causes bronchoconstriction mediated by HI receptors.In the guinea pig,this effect is the cause of death from histamine toxicity,but in humans with normal airways, bronchoconstriction following small doses of histamine is not marked.However, patients with asthma are very sensitive to histamine.The bronchoconstriction induced in these patients probably represents a hyperactive neural response,since such patients also respond excessively to many other stimuli,and the response to histamine can be blocked by autonomic blocking drugs such as ganglionic blocking agents as well as by Hi-receptor antagonists.Although methacholine provocation is more commonly used,tests using increasing doses of inhaled histamine have been used in the diagnosis of bronchial hyperreactivity in patients with suspected asthma or cystic
Presynaptic H3 receptors play important roles in modulating transmitter release in the nervous system. H3 agonists reduce the release of acetylcholine, amine, and peptide transmitters in various areas of the brain and in peripheral nerves. 2. Cardiovascular system In humans, injection or infusion of histamine causes a decrease in systolic and diastolic blood pressure and an increase in heart rate. The blood pressure changes are caused by the direct vasodilator action of histamine on arterioles and precapillary sphincters; the increase in heart rate involves both stimulatory actions of histamine on the heart and a reflex tachycardia. Flushing, a sense of warmth, and headache may also occur during histamine administration, consistent with the vasodilation. Vasodilation elicited by small doses of histamine is caused by H1-receptor activation and is mediated primarily by release of nitric oxide from the endothelium. The decrease in blood pressure is usually accompanied by a reflex tachycardia. Higher doses of histamine activate the H2-mediated cAMP process of vasodilation and direct cardiac stimulation. In humans, the cardiovascular effects of small doses of histamine can usually be antagonized by H1-receptor antagonists alone. Histamine-induced edema results from the action of the amine on H1 receptors in the vessels of the microcirculation, especially the postcapillary vessels. The effect is associated with the separation of the endothelial cells, which permits the transudation of fluid and molecules as large as small proteins into the perivascular tissue. This effect is responsible for the urticaria (hives) that signals the release of histamine in the skin. Studies of endothelial cells suggest that actin and myosin within these cells contract, resulting in separation of the endothelial cells and increased permeability. Direct cardiac effects of histamine include both increased contractility and increased pacemaker rate. These effects are mediated chiefly by H2 receptors. In human atrial muscle, histamine can also decrease contractility; this effect is mediated by H1 receptors. The physiologic significance of these cardiac actions is not clear. Some of the cardiovascular signs and symptoms of anaphylaxis are due to released histamine, though several other mediators are involved and appear to be more important than histamine in humans. 3. Bronchiolar smooth muscle In both humans and guinea pigs, histamine causes bronchoconstriction mediated by H1 receptors. In the guinea pig, this effect is the cause of death from histamine toxicity, but in humans with normal airways, bronchoconstriction following small doses of histamine is not marked. However, patients with asthma are very sensitive to histamine. The bronchoconstriction induced in these patients probably represents a hyperactive neural response, since such patients also respond excessively to many other stimuli, and the response to histamine can be blocked by autonomic blocking drugs such as ganglionic blocking agents as well as by H1-receptor antagonists. Although methacholine provocation is more commonly used, tests using increasing doses of inhaled histamine have been used in the diagnosis of bronchial hyperreactivity in patients with suspected asthma or cystic

fibrosis.Such individuals may be 100-to 1000-fold more sensitive to histamine (and methacholine)than are normal subjects.Curiously,a few species (eg,rabbit)respond to histamine with bronchodilation,reflecting the dominance of the H2 receptor in their airways. 4.Gastrointestinal tract smooth muscle Histamine causes contraction of intestinal smooth muscle,and histamine-induced contraction of guinea pig ileum is a standard bioassay for this amine.The human gut is not as sensitive as that of the guinea pig,but large doses of histamine may cause diarrhea,partly as a result of this effect.This action of histamine is mediated by Hi receptors. 5.Other smooth muscle organs In humans,histamine generally has insignificant effects on the smooth muscle of the eye and genitourinary tract.However,pregnant women suffering anaphylactic reactions may abort as a result of histamine-induced contractions,and in some species the sensitivity of the uterus is sufficient to form the basis for a bioassay. 6.Secretory tissue Histamine has long been recognized as a powerful stimulant of gastric acid secretion and,to a lesser extent,of gastric pepsin and intrinsic factor production.The effect is caused by activation of H2 receptors on gastric parietal cells and is associated with increased adenylyl cyclase activity,cAMP concentration,and intracellular Ca2 concentration.Other stimulants of gastric acid secretion such as acetylcholine and gastrin do not increase cAMP even though their maximal effects on acid output can be reduced but not abolished by H2-receptor antagonists. Histamine also stimulates secretion in the small and large intestine.In contrast, H3-selective histamine agonists inhibit acid secretion stimulated by food or pentagastrin in several species. Histamine has much smaller effects on the activity of other glandular tissue at ordinary concentrations.Very high concentrations can cause adrenal medullary discharge. 7.Metabolic effects Recent studies of H3-receptor knockout mice demonstrate that absence of this receptor results in animals with increased food intake,decreased energy expenditure,and obesity.They also show insulin resistance and increased blood levels of leptin and insulin.It is not yet known whether the H3 receptor has a similar role in humans. 8.The"triple response"Intradermal injection of histamine causes a characteristic red spot,edema,and flare response that was first described over 60 years ago.The effect involves three separate cell types:smooth muscle in the microcirculation, capillary or venular endothelium,and sensory nerve endings.At the site of injection,a reddening appears owing to dilation of small vessels,followed soon by an edematous wheal at the injection site and a red irregular flare surrounding the wheal.The flare is
fibrosis. Such individuals may be 100- to 1000-fold more sensitive to histamine (and methacholine) than are normal subjects. Curiously, a few species (eg, rabbit) respond to histamine with bronchodilation, reflecting the dominance of the H2 receptor in their airways. 4. Gastrointestinal tract smooth muscle Histamine causes contraction of intestinal smooth muscle, and histamine-induced contraction of guinea pig ileum is a standard bioassay for this amine. The human gut is not as sensitive as that of the guinea pig, but large doses of histamine may cause diarrhea, partly as a result of this effect. This action of histamine is mediated by H1 receptors. 5. Other smooth muscle organs In humans, histamine generally has insignificant effects on the smooth muscle of the eye and genitourinary tract. However, pregnant women suffering anaphylactic reactions may abort as a result of histamine-induced contractions, and in some species the sensitivity of the uterus is sufficient to form the basis for a bioassay. 6. Secretory tissue Histamine has long been recognized as a powerful stimulant of gastric acid secretion and, to a lesser extent, of gastric pepsin and intrinsic factor production. The effect is caused by activation of H2 receptors on gastric parietal cells and is associated with increased adenylyl cyclase activity, cAMP concentration, and intracellular Ca2+ concentration. Other stimulants of gastric acid secretion such as acetylcholine and gastrin do not increase cAMP even though their maximal effects on acid output can be reduced but not abolished by H 2-receptor antagonists. Histamine also stimulates secretion in the small and large intestine. In contrast, H3-selective histamine agonists inhibit acid secretion stimulated by food or pentagastrin in several species. Histamine has much smaller effects on the activity of other glandular tissue at ordinary concentrations. Very high concentrations can cause adrenal medullary discharge. 7. Metabolic effects Recent studies of H3-receptor knockout mice demonstrate that absence of this receptor results in animals with increased food intake, decreased energy expenditure, and obesity. They also show insulin resistance and increased blood levels of leptin and insulin. It is not yet known whether the H3 receptor has a similar role in humans. 8. The "triple response" Intradermal injection of histamine causes a characteristic red spot, edema, and flare response that was first described over 60 years ago. The effect involves three separate cell types: smooth muscle in the microcirculation, capillary or venular endothelium, and sensory nerve endings. At the site of injection, a reddening appears owing to dilation of small vessels, followed soon by an edematous wheal at the injection site and a red irregular flare surrounding the wheal. The flare is
said to be caused by an axon reflex.A sensation of itching may accompany these effects. Similar local effects may be produced by injecting histamine liberators(compound 48/80,morphine,etc)intradermally or by applying the appropriate antigens to the skin of a sensitized person.Although most of these local effects can be blocked by prior administration of an Hi-receptor-blocking agent,H2 and H3 receptors may also be involved. 9.Other effects possibly mediated by histamine receptors In addition to the local stimulation of peripheral pain nerve endings via H3 and HI receptors,histamine may play a role in nociception in the central nervous system.Burimamide,an early candidate for H2 blocking action,and newer analogs with no effect on Hi,H2,or H3 receptors,have been shown to have significant analgesic action in rodents when administered into the central nervous system.The analgesia is said to be comparable to that produced by opioids,but tolerance,respiratory depression,and constipation have not been reported.Although the mechanism of this action is not known,these compounds may represent an important new class of analgesics. Other Histamine Agonists Small substitutions on the imidazole ring of histamine significantly modify the selectivity of the compounds for the histamine receptor subtypes. CLINICAL PHARMACOLOGY OF HISTAMINE Clinical Uses In pulmonary function laboratories,histamine aerosol has been used as a provocative test of bronchial hyperreactivity.Histamine has no other current clinical applications. Toxicity Contraindications Adverse effects of histamine release,like those following administration of histamine, are dose-related.Flushing,hypotension,tachycardia,headache,wheals, bronchoconstriction,and gastrointestinal upset are noted.These effects are also observed after the ingestion of spoiled fish(scombroid fish poisoning),and there is evidence that histamine produced by bacterial action in the flesh of the fish is the major causative agent. Histamine should not be given to patients with asthma(except as part of a carefully monitored test of pulmonary function)or to patients with active ulcer disease or gastrointestinal bleeding
said to be caused by an axon reflex. A sensation of itching may accompany these effects. Similar local effects may be produced by injecting histamine liberators (compound 48/80, morphine, etc) intradermally or by applying the appropriate antigens to the skin of a sensitized person. Although most of these local effects can be blocked by prior administration of an H1-receptor-blocking agent, H2 and H3 receptors may also be involved. 9. Other effects possibly mediated by histamine receptors In addition to the local stimulation of peripheral pain nerve endings via H3 and H1 receptors, histamine may play a role in nociception in the central nervous system. Burimamide, an early candidate for H2 blocking action, and newer analogs with no effect on H1, H2, or H3 receptors, have been shown to have significant analgesic action in rodents when administered into the central nervous system. The analgesia is said to be comparable to that produced by opioids, but tolerance, respiratory depression, and constipation have not been reported. Although the mechanism of this action is not known, these compounds may represent an important new class of analgesics. Other Histamine Agonists Small substitutions on the imidazole ring of histamine significantly modify the selectivity of the compounds for the histamine receptor subtypes. CLINICAL PHARMACOLOGY OF HISTAMINE Clinical Uses In pulmonary function laboratories, histamine aerosol has been used as a provocative test of bronchial hyperreactivity. Histamine has no other current clinical applications. Toxicity Contraindications Adverse effects of histamine release, like those following administration of histamine, are dose-related. Flushing, hypotension, tachycardia, headache, wheals, bronchoconstriction, and gastrointestinal upset are noted. These effects are also observed after the ingestion of spoiled fish (scombroid fish poisoning), and there is evidence that histamine produced by bacterial action in the flesh of the fish is the major causative agent. Histamine should not be given to patients with asthma (except as part of a carefully monitored test of pulmonary function) or to patients with active ulcer disease or gastrointestinal bleeding

HISTAMINE ANTAGONISTS The effects of histamine released in the body can be reduced in several ways. Physiologic antagonists,especially epinephrine,have smooth muscle actions opposite to those of histamine,but they act at different receptors.This is important clinically because injection of epinephrine can be lifesaving in systemic anaphylaxis and in other conditions in which massive release of histamine and other mediators occurs. Release inhibitors reduce the degranulation of mast cells that results from immunologic triggering by antigen-IgE interaction.Cromolyn and nedocromil appear to have this effect and are used in the treatment of asthma,though the molecular mechanism underlying their action is presently unknown.Beta2-adrenoceptor agonists also appear capable of reducing histamine release. Histamine receptor antagonists represent a third approach to the reduction of histamine-mediated responses.For over 60 years,compounds have been available that competitively antagonize many of the actions of histamine on smooth muscle. However,not until the H2-receptor antagonist burimamide was described in 1972 was it possible to antagonize the gastric acid-stimulating activity of histamine.The development of selective H2-receptor antagonists has led to more effective therapy for peptic disease.Selective H3 and H4 antagonists are not yet available for clinical use. However,potent and selective experimental H3-receptor antagonists,thioperamide and clobenpropit,have been developed. PREPARATIONS AVAILABLE ANTIHISTAMINES (H BLOCKERS)* Azelastine Nasal (Astelin):137 mcg/puff nasal spray Ophthalmic (Optivar):0.5 mg/mL solution Brompheniramine(generic,Brovex) Oral:6,12 mg extended release tablets;12 mg chewable tablets;8,12 mg/5 mL suspension Buclizine(Bucladin-S Softabs) Oral:50 mg tablets Carbinoxamine(Histex,Pediatex) Oral:4 mg tablets;8 mg timed-release tablets;10 mg extended release capsules; 1.5,4 mg/5 mL liquid;3.6 mg/5 mL oral suspension Cetirizine(Zyrtec) Oral:5,10 mg tablets;5,10 mg chewable tablets;5 mg/5 mL syrup
HISTAMINE ANTAGONISTS The effects of histamine released in the body can be reduced in several ways. Physiologic antagonists, especially epinephrine, have smooth muscle actions opposite to those of histamine, but they act at different receptors. This is important clinically because injection of epinephrine can be lifesaving in systemic anaphylaxis and in other conditions in which massive release of histamine and other mediators occurs. Release inhibitors reduce the degranulation of mast cells that results from immunologic triggering by antigen-IgE interaction. Cromolyn and nedocromil appear to have this effect and are used in the treatment of asthma, though the molecular mechanism underlying their action is presently unknown. Beta2-adrenoceptor agonists also appear capable of reducing histamine release. Histamine receptor antagonists represent a third approach to the reduction of histamine-mediated responses. For over 60 years, compounds have been available that competitively antagonize many of the actions of histamine on smooth muscle. However, not until the H2-receptor antagonist burimamide was described in 1972 was it possible to antagonize the gastric acid-stimulating activity of histamine. The development of selective H2-receptor antagonists has led to more effective therapy for peptic disease. Selective H3 and H4 antagonists are not yet available for clinical use. However, potent and selective experimental H3-receptor antagonists, thioperamide and clobenpropit, have been developed. PREPARATIONS AVAILABLE ANTIHISTAMINES (H1 BLOCKERS)* Azelastine Nasal (Astelin): 137 mcg/puff nasal spray Ophthalmic (Optivar): 0.5 mg/mL solution Brompheniramine (generic, Brovex) Oral: 6, 12 mg extended release tablets; 12 mg chewable tablets; 8, 12 mg/5 mL suspension Buclizine (Bucladin-S Softabs) Oral: 50 mg tablets Carbinoxamine (Histex, Pediatex) Oral: 4 mg tablets; 8 mg timed-release tablets; 10 mg extended release capsules; 1.5, 4 mg/5 mL liquid; 3.6 mg/5 mL oral suspension Cetirizine (Zyrtec) Oral: 5, 10 mg tablets; 5, 10 mg chewable tablets; 5 mg/5 mL syrup

Chlorpheniramine(generic,Chlor-Trimeton) Oral:2 mg chewable tablets;4 mg tablets;2 mg/5 mL syrup Oral sustained-release:8,12,16 mg tablets;8,12 mg capsules Clemastine(generic,Tavist) Oral:1.34,2.68 mg tablets;0.67 mg/5 mL syrup Cyclizine (Marezine) Oral:50 mg tablets Cyproheptadine(generic) Oral:4 mg tablets;2 mg/5 mL syrup Desloratadine(Clarinex) Oral:5 mg regular or rapidly disintegrating tablets;2.5 mg/5 mL syrup Dexchlorpheniramine(generic) Oral:4,6 mg extended release tablets;2 mg/5 mL syrup Dimenhydrinate (Dramamine,others) Oral:50 mg tablets;50 mg chewable tablets;12.5/5 mL,12.5 mg/4 mL,15.62 mg/5 mL liquid Parenteral:50 mg/mL for IM or IV injection Diphenhydramine(generic,Benadryl) Oral:12.5 mg chewable tablets;25,50 mg tablets,capsules;12.5 mg/5 mL elixir and syrup Parenteral:50 mg/mL for injection Emedastine(Emadine) Ophthalmic:0.05%solution Epinastine(Elestat) Ophthalmic:0.05%solution Fexofenadine(Allegra) Oral:30,60,180 mg tablets;60 mg capsules Hydroxyzine(generic,Vistaril) Oral:10,25,50 mg tablets;25,50,100 mg capsules;10 mg/5 mL syrup;25 mg/5 mL suspension Parenteral:25,50 mg/mL for injection Ketotifen (Zaditor) Ophthalmic:0.025%solution Levocabastine (Livostin) Ophthalmic:0.05%solution Loratadine (generic,Claritin,Tavist) Oral:10 mg tablets;10 mg rapidly disintegrating tablets;1 mg/mL syrup Meclizine(generic,Antivert) Oral:12.5,25,50 mg tablets;25 mg capsules;25 mg chewable tablets Olopatadine (Patanol) Ophthalmic:0.1%solution Phenindamine (Nolahist) Oral:25 mg tablets
Chlorpheniramine (generic, Chlor-Trimeton) Oral: 2 mg chewable tablets; 4 mg tablets; 2 mg/5 mL syrup Oral sustained-release: 8, 12, 16 mg tablets; 8, 12 mg capsules Clemastine (generic, Tavist) Oral: 1.34, 2.68 mg tablets; 0.67 mg/5 mL syrup Cyclizine (Marezine) Oral: 50 mg tablets Cyproheptadine (generic) Oral: 4 mg tablets; 2 mg/5 mL syrup Desloratadine (Clarinex) Oral: 5 mg regular or rapidly disintegrating tablets; 2.5 mg/5 mL syrup Dexchlorpheniramine (generic) Oral: 4, 6 mg extended release tablets; 2 mg/5 mL syrup Dimenhydrinate (Dramamine, others) Oral: 50 mg tablets; 50 mg chewable tablets; 12.5/5 mL, 12.5 mg/4 mL, 15.62 mg/5 mL liquid Parenteral: 50 mg/mL for IM or IV injection Diphenhydramine (generic, Benadryl) Oral: 12.5 mg chewable tablets; 25, 50 mg tablets, capsules; 12.5 mg/5 mL elixir and syrup Parenteral: 50 mg/mL for injection Emedastine (Emadine) Ophthalmic: 0.05% solution Epinastine (Elestat) Ophthalmic: 0.05% solution Fexofenadine (Allegra) Oral: 30, 60, 180 mg tablets; 60 mg capsules Hydroxyzine (generic, Vistaril) Oral: 10, 25, 50 mg tablets; 25, 50, 100 mg capsules; 10 mg/5 mL syrup; 25 mg/5 mL suspension Parenteral: 25, 50 mg/mL for injection Ketotifen (Zaditor) Ophthalmic: 0.025% solution Levocabastine (Livostin) Ophthalmic: 0.05% solution Loratadine (generic, Claritin, Tavist) Oral: 10 mg tablets; 10 mg rapidly disintegrating tablets; 1 mg/mL syrup Meclizine (generic, Antivert) Oral: 12.5, 25, 50 mg tablets; 25 mg capsules; 25 mg chewable tablets Olopatadine (Patanol) Ophthalmic: 0.1% solution Phenindamine (Nolahist) Oral: 25 mg tablets