1/26/2016 Antimicrobial drugs act by inhibiting or Microbes interfering with the growth of microbes. .Antimicrobial drugs act within the host without damaging the host. Invisible Invaders Antibiotics are one of the most important Amazing Allies discoveries of modern medicine. Resistance to antibiotics poses a "major global threat"to public health according to WHO. Chapter 20 Antimicrobial Drugs The History of Chemotherapy The History of Chemotherapy x:selectively finding and Learning Objectives stroying pathogens without damaging the host Identify the contributions of Paul Ehrlich and the use of chemicals to Alexander Fleming to chemotherapy. Name the microbes that produce most Antibiotic:a substance produced by a antibiotics. microbe that,in small amounts,inhibits another microbe microbes
1/26/2016 1 Invisible Invaders Amazing Allies Chapter 20 Antimicrobial Drugs • Antimicrobial drugs act by inhibiting or interfering with the growth of microbes. • Antimicrobial drugs act within the host without damaging the host. • Antibiotics are one of the most important discoveries of modern medicine. • Resistance to antibiotics poses a "major global threat" to public health according to WHO. Pseudomonas aeruginosa resistant to many antibiotics The History of Chemotherapy Learning Objectives Identify the contributions of Paul Ehrlich and Alexander Fleming to chemotherapy. Name the microbes that produce most antibiotics. The History of Chemotherapy • Selective toxicity: selectively finding and destroying pathogens without damaging the host • Chemotherapy: the use of chemicals to treat a disease • Antibiotic: a substance produced by a microbe that, in small amounts, inhibits another microbe • Antimicrobial drugs: synthetic substances that interfere with the growth of microbes
1/26/2016 The History of Chemotherapy The History of Chemotherapy ·8ec8ee8¥Y .1928:Fleming discovered penicillin, Ehrlich,Germany produced by Penicillium ·be8 oul e 1932:Prontosil red dye used for streptococcal infections horr pathager but 1940:First clinical trials of penicillin Father of chemotherapy Today there is a growing problem of antibiotic resistance %gea25米t "One sometimes finds what one is ·Nobel prize in1908 ot looking for." Alexander Fleming TABLE 20.7 Representative Sources of Antibiotics cieifn8m5mbncsie2alteiera Microorganism Antibiotic GRAM-POSITIVE RODS Most commonly Streptomyces species B联nan Polymyrin ACTINOMYCETES FUNGI
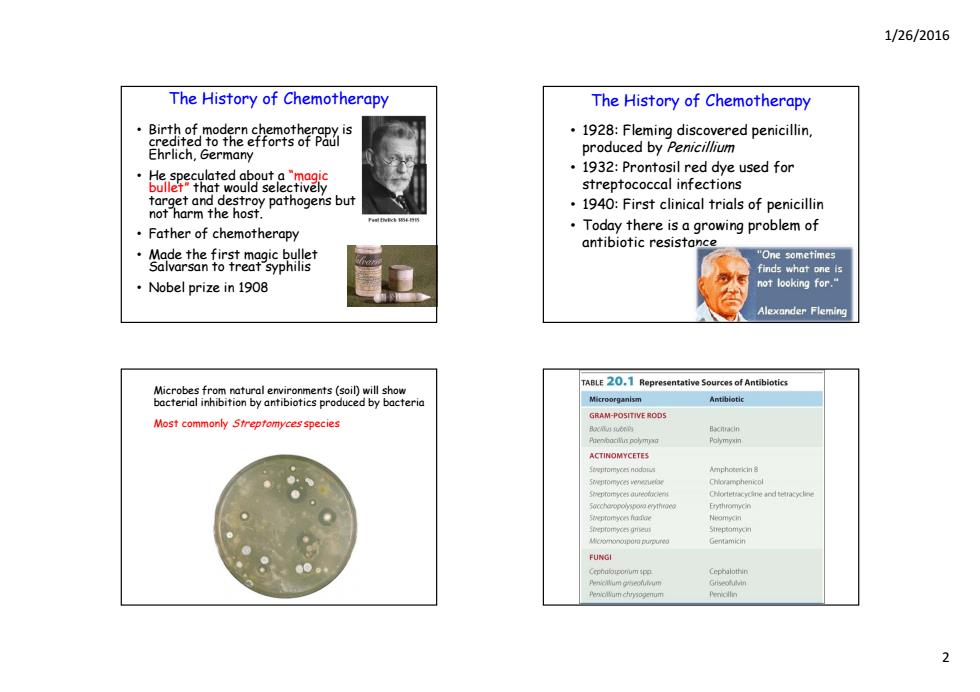
1/26/2016 2 The History of Chemotherapy • Birth of modern chemotherapy is credited to the efforts of Paul Ehrlich, Germany • He speculated about a “magic bullet” that would selectively target and destroy pathogens but not harm the host. • Father of chemotherapy • Made the first magic bullet Salvarsan to treat syphilis • Nobel prize in 1908 The History of Chemotherapy • 1928: Fleming discovered penicillin, produced by Penicillium • 1932: P t sil d d s d f 1932: Prontosil red dye used for streptococcal infections • 1940: First clinical trials of penicillin • Today there is a growing problem of antibiotic resistance Microbes from natural environments (soil) will show bacterial inhibition by antibiotics produced by bacteria Most commonly Streptomyces species
1/26/2016 Spectrum of Antimicrobial Activity Spectrum of Antimicrobial Activity Selective toxicity has Learning Objectives numerous fargets for drug development for prokaryotes Describe the problems of chemotherapy for viral,fungal,protozoan,and helminthic Cell structure of eukaryotes infections. is very similar to that of the human host Define the following terms:spectrum of activity,broad-spectrum antibiotic, Viruses multiply within the Superinfection. host cell. Selective toxicity is more difficult for viruses and eukaryotic pathogens. The Spectrum of Activity of Antibiotics and Other Antimicrobial Drugs Spectrum of Antimicrobial Activity Narrow spectrum of microbial activity:drugs that affect a narrow range of microbial types Antibiotics target the normal flora as well as the pathogen. tive bacteria Survivors may flourish and become opportuntistic pathogens due to overgrowth. Superinfection:overgrowth of normal microbiota that is resistant to antibiotics
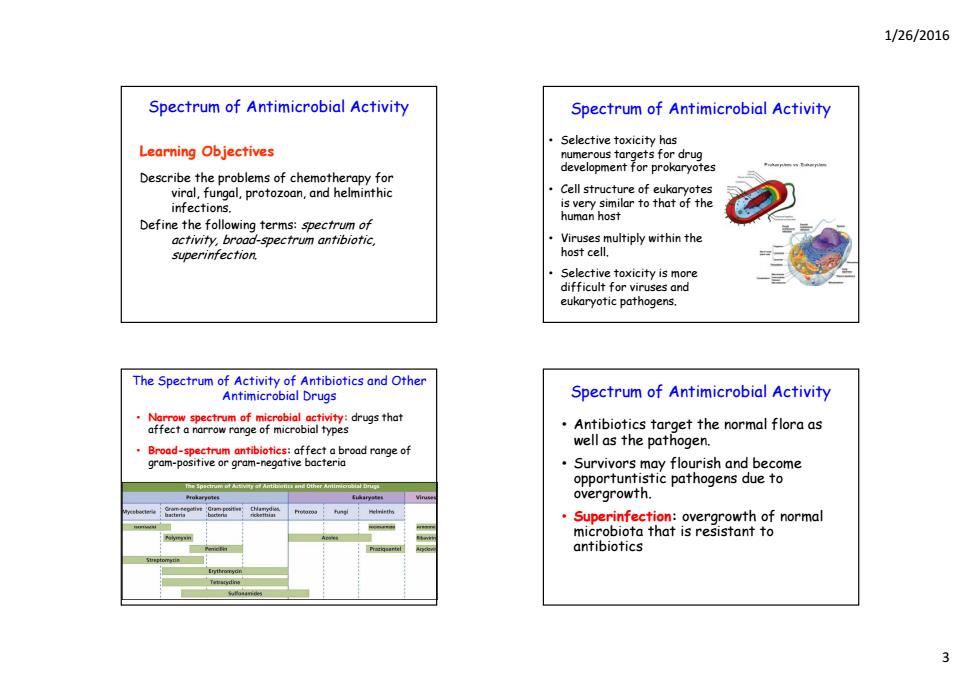
1/26/2016 3 Spectrum of Antimicrobial Activity Learning Objectives Describe the problems of chemotherapy for viral, fungal, protozoan, and helminthic infections. Define the following terms: spectrum of activity, broad-spectrum antibiotic, superinfection. Spectrum of Antimicrobial Activity • Selective toxicity has numerous targets for drug d l t f k t development for prokaryotes • Cell structure of eukaryotes is very similar to that of the human host • Viruses multip yl within the host cell. • Selective toxicity is more difficult for viruses and eukaryotic pathogens. The Spectrum of Activity of Antibiotics and Other Antimicrobial Drugs • Narrow spectrum of microbial activity: drugs that affect a narrow range of microbial types • B d roa -spect tibi ti trum antibiotics: aff t b d f ffect a broad range of gram-positive or gram-negative bacteria Spectrum of Antimicrobial Activity • Antibiotics target the normal flora as well as the p g atho en. • Survivors may flourish and become opportuntistic pathogens due to overgrowth. • Superinfection: overgrowth of normal mi bi h i i icrobiota that is resistant to antibiotics
1/26/2016 The Action of Antimicrobial Drugs The Action of Antimicrobial Drugs ·Bactericidal Learning Objective -Kill microbes directly Identify five modes of action of antimicrobial Bacteriostatic drugs. -Prevent microbes from growing -Host's immune system usually kills the pathogen Five Major Targets of Antibacterial Drugs Antimicrobial drugs target essential functions of the microbe The Action of Antimicrobial Drugs Inhibiting cell wall synthesis -Peptidoglycan is found only in bacterial cell walls. -Penicillins prevent the synthesis of peptidoglycan -Cell wall is weakened and undergoes lysis. ma embran
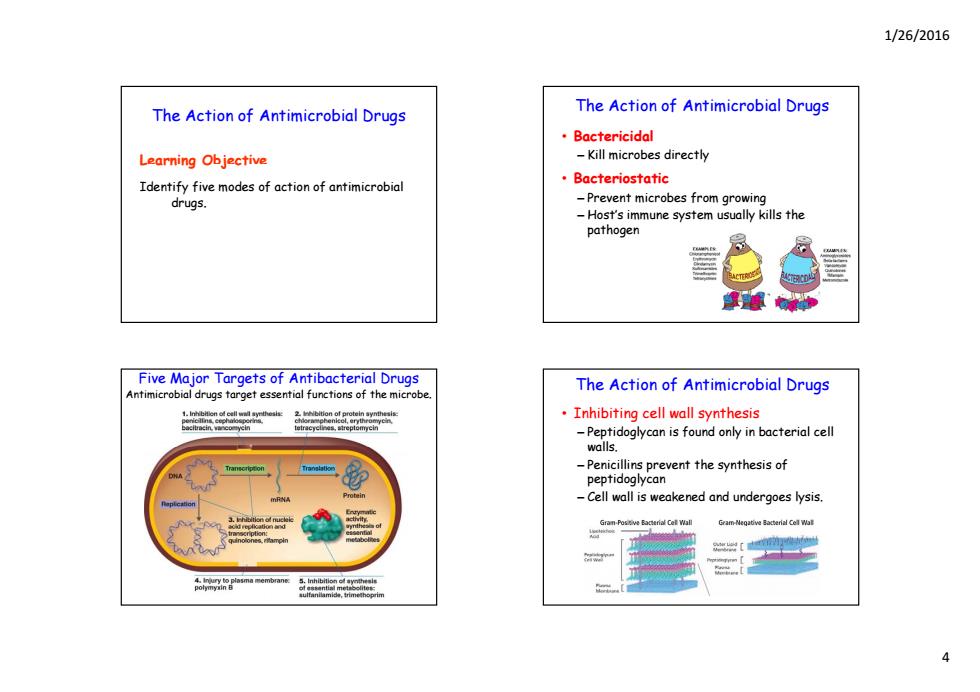
1/26/2016 4 The Action of Antimicrobial Drugs L arn ng O j ct earning Objective Identify five modes of action of antimicrobial drugs. The Action of Antimicrobial Drugs • Bactericidal – Kill microbes directly • Bacteriostatic – Prevent microbes from growing – Host’s immune system usually kills the pathogen Five Major Targets of Antibacterial Drugs Antimicrobial drugs target essential functions of the microbe. The Action of Antimicrobial Drugs • Inhibiting cell wall synthesis – Peptidoglycan is found only in bacterial cell walls. – Penicillins prevent the synthesis of peptidoglycan – Cell wall is weakened and undergoes lysis

1/26/2016 Inhibition of bacterial cell wall synthesis by The Action of Antimicrobial Drugs penicillin Inhibiting protein synthesis -Target bacterial 70S ribosomes -Eukaryotes have 805 ribosomes -Difference in ribosome structure accounts for selective toxicity -However,mitochondria have 705 ribosomes 四1m The ba so some toxicity may occur -Chloramphenicol,erythromycin, streptomycin,tetracyclines Protein synthesis Inhibition of protein synthesis by antibiotics. Growing polypeptide nthesis nd inhibits site -Protein synthesis site ortse Totracyclines hh8r2e8s305ay nges shape of Interfere with Translation RNA to mRNA- bosome comple
1/26/2016 5 Inhibition of bacterial cell wall synthesis by penicillin The Action of Antimicrobial Drugs • Inhibiting protein synthesis – Target bacterial 70S ribosomes – Eukaryotes have 80S ribosomes – Difference in ribosome structure accounts for selective toxicity – However, mitochondria have 70S ribosomes so t i it some toxicit y may occur – Chloramphenicol, erythromycin, streptomycin, tetracyclines Protein synthesis Protein synthesis site Growing polypeptide Tunnel 5' 50S 30S mRNA 3' Three-dimensional detail of the protein synthesis site showing the 30S and 50S subunit portions of the 70S prokaryotic ribosome Inhibition of protein synthesis by antibiotics. Growing polypeptide 50S Chloramphenicol Binds to 50S portion and inhibits formation of tid b d Messenger RNA 50S portion tRNA Protein synthesis site peptide bond RNA Streptomycin Changes shape of 30S portion, causing code on mRNA to be read incorrectly 70S prokaryotic ribosome Translation 30S portion Direction of ribosome movement Tetracyclines Interfere with attachment of tRNA to mRNA– ribosome complex
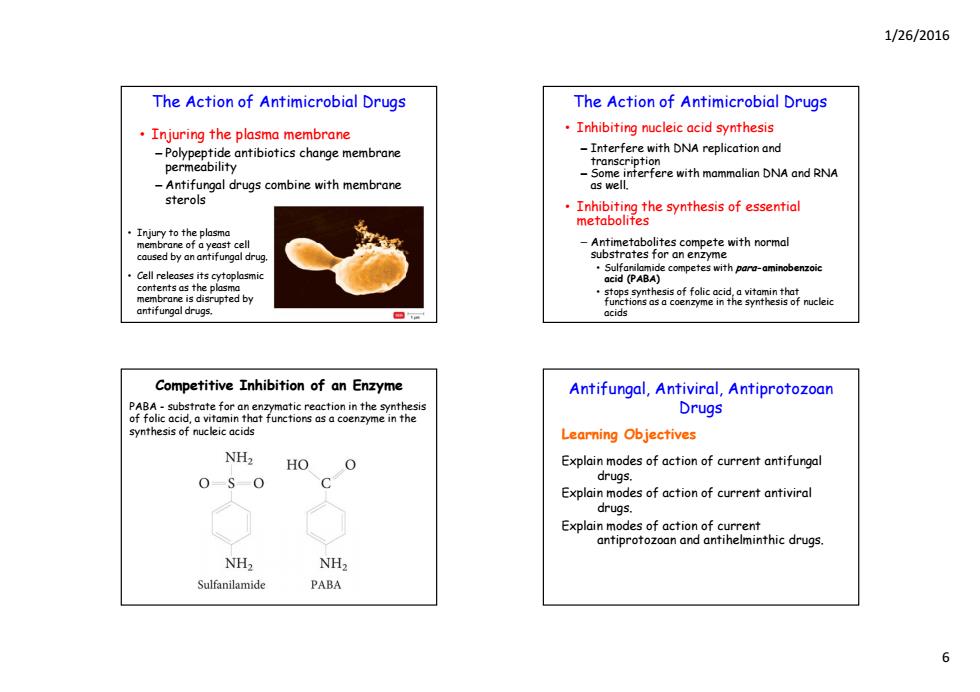
1/26/2016 The Action of Antimicrobial Drugs The Action of Antimicrobial Drugs Injuring the plasma membrane Inhibiting nucleic acid synthesis -Polypeptide antibiotics change membrane -Interfere with DNA replication and permeability transcription Some interfere with mammalian DNA and RNA -Antifungal drugs combine with membrane as well. sterols .Inhibiting the synthesis of essential metabolites ·Injury to the plasma membrane of a yeast cell caused by an antifungal drug. trates for an enzyme Cell releases its cytoplasmic competeprminbenie contents as the plasma membrane is disrupted by ions as a coenzyme in antifungal drugs. Competitive Inhibition of an Enzyme Antifungal,Antiviral,Antiprotozoan PABA-substrate for an enzymatic reaction in the synthesis of folic acid,a vitamin that functions as a coenzyme in the Drugs synthesis of nucleic acids Learning Objectives NH2 HO O Explain modes of action of current antifungal 0-S0 C drugs. Explain modes of action of current antiviral drugs. Explain modes of action of current antiprotozoan and antihelminthic drugs. NH2 NH2 Sulfanilamide PABA 6
1/26/2016 6 The Action of Antimicrobial Drugs • Injuring the plasma membrane – Polypeptide antibiotics change membrane p m bilit permeability – Antifungal drugs combine with membrane sterols • Injury to the plasma membrane of a yeast cell caused by an antifungal drug. • Cell releases its cytoplasmic contents as the plasma membrane is disrupted by antifungal drugs. The Action of Antimicrobial Drugs • Inhibiting nucleic acid synthesis – Interfere with DNA replication and transcr transcr pt on i i – Some interfere with mammalian DNA and RNA as well. • Inhibiting the synthesis of essential metabolites – Antimetabolites compete with normal substrates for an enzyme • Sulfanilamide competes with para-aminobenzoic acid (PABA) • stops synthesis of folic acid, a vitamin that functions as a coenzyme in the synthesis of nucleic acids Competitive Inhibition of an Enzyme PABA - substrate for an enzymatic reaction in the synthesis of folic acid, a vitamin that functions as a coenzyme in the synthesis of nucleic acids Antifungal, Antiviral, Antiprotozoan Drugs Learning Objectives Explain modes of action of current antifungal drugs. Explain modes of action of current antiviral drugs. Explain modes of action of current antiprotozoan and antihelminthic drugs
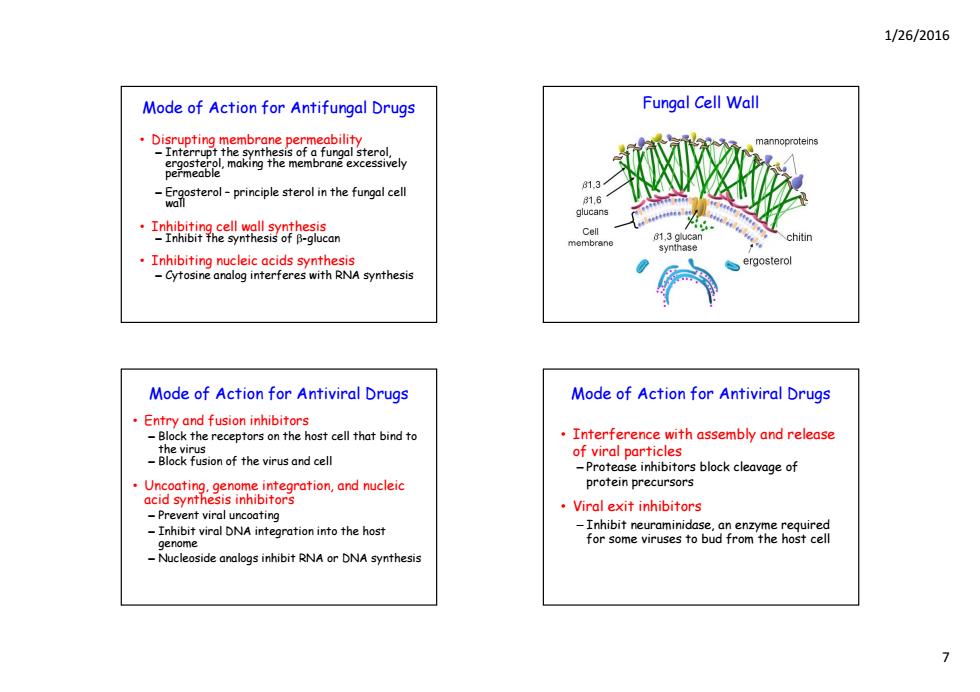
1/26/2016 Mode of Action for Antifungal Drugs Fungal Cell Wall oal sterol. mannoproteins 81.3 tero-principle sterol in the fungal cell 1日 Inhibiting cell wall synthesis -Inhibit the synthesis of B-glucan Cell chitin Inhibiting nucleic acids synthesis ergosterol -Cytosine analog interferes with RNA synthesis Mode of Action for Antiviral Drugs Mode of Action for Antiviral Drugs Entry and fusion inhibitors -Block the receptors on the host cell that bind to Interference with assembly and release the virus -Block fusion of the virus and cell of viral particles -Protease inhibitors block cleavage of Uncoating.genome integration,and nucleic protein precursors acid synthesis inhibitors Viral exit inhibitors -Prevent viral uncoating Inhibit viral DNA integration into the host -Inhibit neuraminidase,an enzyme required genome for some viruses to bud from the host cell -Nucleoside analogs inhibit RNA or DNA synthesis >
1/26/2016 7 Mode of Action for Antifungal Drugs • Disrupting membrane permeability – Interrupt the synthesis of a fungal sterol, ergosterol making the membrane excessively ergosterol, making the membrane excessively permeable – Ergosterol – principle sterol in the fungal cell wall • Inhibiting cell wall synthesis – Inhibit the synthesis of -glucan • Inhibiting nucleic acids synthesis – Cytosine analog interferes with RNA synthesis Fungal Cell Wall • Entry and fusion inhibitors – Block the receptors on the host cell that bind to the virus Mode of Action for Antiviral Drugs – Block fusion of the virus and cell • Uncoating, genome integration, and nucleic acid synthesis inhibitors – Prevent viral uncoating – I hibi i l DNA i i i h h Inhibit viral DNA integration into the host genome – Nucleoside analogs inhibit RNA or DNA synthesis • Interference with assembly and release f i l ti l Mode of Action for Antiviral Drugs of viral particles – Protease inhibitors block cleavage of protein precursors • Viral exit inhibitors – Inhibit neuraminidase an enzyme required Inhibit neuraminidase, an enzyme required for some viruses to bud from the host cell

1/26/2016 Replication of a Virus Structure and function of the antiviral drug acyclovir Guanine sembly s the nu Mode of Action for Antiprotozoan S ONA and Antihelminthic Drugs AXX Many antiprotozoan and antihelminthic drugs cleosides to form are available now but are considered still experimental. Phosphate 关 One malarial drug targets the asexual stages of Plasmodium,which causes malaria (aev5aat间 Another protozoan drug interferes with anaerobic respiration,which is similar to dovir has no effect ona cell not infected by a yirus. that in bacteria,and works on obligate anaerobic bacteria as well
1/26/2016 8 Replication of a Virus Structure and function of the antiviral drug acyclovir Guanine Acyclovir structurally resembles the nucleoside deoxyguanosine. Deoxyguanosine Acyclovir Phosphate Nucleoside Guanine nucleotide Host thymidine kinase DNA polymerase Incorporated into DNA Phosphate DNA polymerase blocked by false nucleotide. Assembly of DNA stops. Acyclovir Viral-encoded thymidine kinase Thymidine kinase combines phosphates with nucleosides to form nucleotides, which are incorporated into DNA. False nucleotide (acyclovir triphosphate) Acyclovir (resembles nucleoside) •Acyclovir has no effect on a cell not infected by a virus. •In a virally infected cell, the thymidine kinase is altered and converts the acyclovir to a false nucleotide, which blocks DNA synthesis by DNA polymerase. Many antiprotozoan and antihelminthic drugs are available now but are considered still Mode of Action for Antiprotozoan and Antihelminthic Drugs experimental. • One malarial drug targets the asexual stages of Plasmodium, which causes malaria • Another protozoan drug interferes with anaerobic respiration, which is similar to that in bacteria, and works on obligate anaerobic bacteria as well
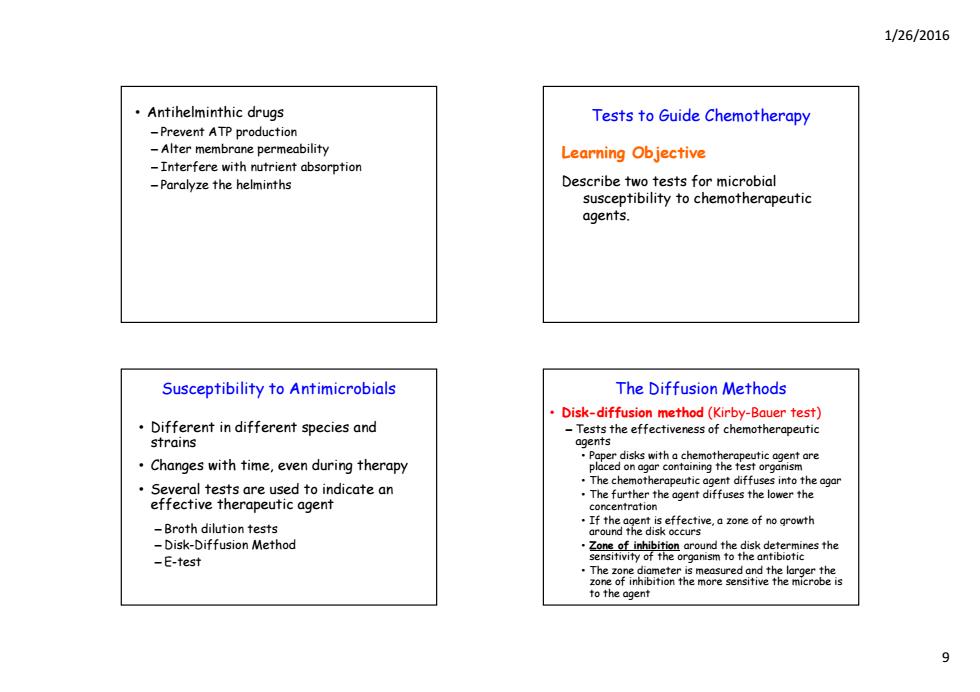
1/26/2016 Antihelminthic drugs Tests to Guide Chemotherapy -Prevent ATP production -Alter membrane permeability Learning Objective -Interfere with nutrient absorption -Paralyze the helminths Describe two tests for microbial susceptibility to chemotherapeutic agents. Susceptibility to Antimicrobials The Diffusion Methods Disk-diffusion method(Kirby-Bauer test) Different in different species and -Tests the effectiveness of chemotherapeutic strains agents Changes with time,even during therapy Several tests are used to indicate an The chemotherapeutic agent diffuses into the agar effective therapeutic agent The further the agent diffuses the lower the concentration -Broth dilution tests If the agent is effective,a zone of no growth around the disk occurs -Disk-Diffusion Method -E-test to the agent
1/26/2016 9 • Antihelminthic drugs – Prevent ATP production – Alter membrane permeability – Interfere with nutrient absorption – Paralyze the helminths Tests to Guide Chemotherapy Learning Objective Describe two tests for microbial susceptibility to chemotherapeutic agents. Susceptibility to Antimicrobials • Different in different species and stra ns i • Changes with time, even during therapy • Several tests are used to indicate an effective therapeutic agent – B th dil ti t sts Broth dilution tests – Disk-Diffusion Method – E-test The Diffusion Methods • Disk-diffusion method (Kirby-Bauer test) – Tests the effectiveness of chemotherapeutic agents • Paper disks with a chemotherapeutic agent are placed on agar containing the test organism • The chemotherapeutic agent diffuses into the agar • The further the agent diffuses the lower the concentration • If the agent is effective, a zone of no growth around the disk occurs • Zone of inhibition around the disk determines the sensitivity of the organism to the antibiotic • The zone diameter is measured and the larger the zone of inhibition the more sensitive the microbe is to the agent

1/26/2016 Disk-diffusion method for determining the The Diffusion Methods activity of antimicrobials. ·Disks containing antimicrobials are ·E test placed on a lawn of bacterial growth -Determines the minimal inhibitory ·Plates are incubated concentration (MIC) for a standardized time Lowest antibiotic concentration that Zone of inhibition is prevents visible bacterial growth e epe .A plastic coated strip contains a gradient of antibiotic concentrations sensitivity as The MIC is read from a scale printed on the -Sensitive strip -Intermediate -Resistant Etest(for epsilometer).a gradient diffusion method that determines antibiotic sensitivity and estimates Broth Dilution Tests minimal inhibitory concentration (MIC) Determine the MIC and minimal bactericidal concentration (MBC)of an antimicrobial drug Test organism is placed into the wells of a tray containing decreasing concentrations of a drug ·Growth is determined cedrg-rmdemeif red in drug-fre ermine if ·Antibiograms -Reports that record the susceptibility of organisms encountered clinically 10
1/26/2016 10 Disk-diffusion method for determining the activity of antimicrobials. • Disks containing antimicrobials are placed on a lawn of bacterial growth • Plates are incubated for a standardized time • Zone of inhibition is compared to a standard table that reports the sensitivity as ─ Sensitive ─ Intermediate ─ Resistant The Diffusion Methods • E test – Determines the minimal inhibitory concentration (MIC) • Lowest antibiotic concentration that prevents visible bacterial growth • A plastic coated strip contains a gradient of antibi i i ibiotic concentrations • The MIC is read from a scale printed on the strip E test (for epsilometer), a gradient diffusion method that determines antibiotic sensitivity and estimates minimal inhibitory concentration (MIC) MIC Broth Dilution Tests • Determine the MIC and minimal bactericidal concentration (MBC) of an antimicrobial drug • Test organism is placed into the wells of a tray containing decreasing concentrations of a drug • Growth is determined • The wells that do not show growth may be cultured in drug-free medium to determine if th d u is the drug is b ct icid l bactericidal or b ct i st tic bacteriostatic. • Antibiograms – Reports that record the susceptibility of organisms encountered clinically