1/26/2016 Microbes Infectious diseases of the brain and spinal cord are devastating Damage leads to deafness. Invisible Invaders blindness,learning disabilities,paralysis,and Amazing Allies death Blood-brain barrier protects these areas Pathogens have special Chapter 22 factors that allo them to Naegleria fowlerian Microbial Diseases of the Nervous penetrate this defense ameba(red)in human brain tissue:enters the brain via System an olfactory nerve Structure and Function of the Structure and Function of the Nervous Nervous System System Two divisions: Learning Objectives Central nervous system(CNS):brain and spinal Define central nervous system and blood- cord -Control center for the body brain barrier. Peripheral nervous system(PNS):nerves that Differentiate meningitis from branch from the CNS encephalitis. -Lines of communication in the body Meninges protect the brain and spinal cord -Three continuous membrane layers Blood-brain barrier cell membranes allow certain substances to pass but restrict others
1/26/2016 1 Invisible Invaders Amazing Allies Chapter 22 Microbial Diseases of the Nervous System • Infectious diseases of the brain and spinal cord are devastating • Damage leads to deafness, blindness, learning disabilities, paralysis, and death • Blood-brain barrier protects these areas Naegleria fowleri an ameba (red) in human brain tissue; enters the brain via an olfactory nerve • Pathogens have special factors that allow them to penetrate this defense Structure and Function of the Nervous System Learning Objectives Define central nervous system and blood– brain barrier. Differentiate meningitis from encephalitis. Structure and Function of the Nervous System Two divisions: • Central nervous system (CNS): brain and spinal cord - Control center for the body • Peripheral nervous system (PNS): nerves that branch from the CNS - Lines of communication in the body • Meninges protect the brain and spinal cord – Three continuous membrane layers • Blood–brain barrier cell membranes allow certain substances to pass but restrict others
1/26/2016 The meninges and cerebrospinal fluid Structure and Function of the Nervous System Skull bone Cerebrum ura mater Meningitis:inflammation of the oid mater meninges Pia mate Encephalitis:inflammation of the brain Cerebrum Meningoencephalitis:inflammation of Blood vessel both Pia mater Subarachnoid s Central cn(crd) Bacterial Diseases of the Nervous System Bacterial Diseases of the Nervous System Learning Objectives Learning Objectives Discuss the epidemiology of meningitis Discuss the epidemiology of tetanus, caused by Haemophilus influenzae, including mode of transmission,etiology. Neisseria meningitidis,Streptococcus disease symptoms,and preventive pneumoniae,and Listeria measures. monocytogenes. State the causative agent,symptoms, Explain how bacterial meningitis is suspect foods,and treatment for diagnosed and treated. botulism
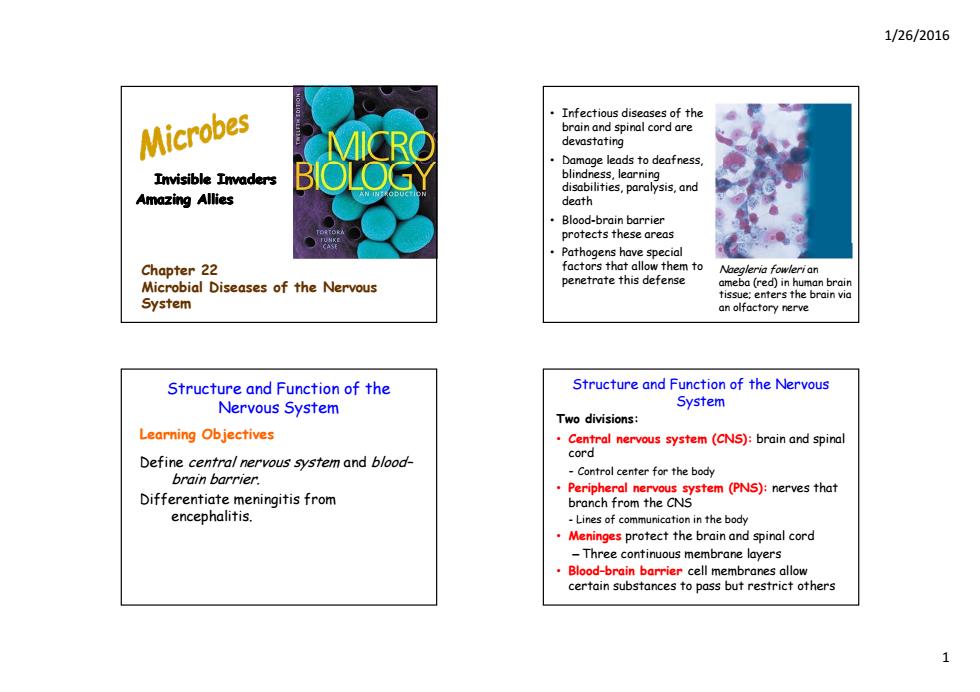
1/26/2016 2 The meninges and cerebrospinal fluid Cerebrum Subarachnoid space (contains cerebrospinal fluid) Skull bone Dura mater Skull bone Arachnoid mater Pia mater Blood vessel Cerebrum Cranial meninges D t Cerebellum Dura mater Arachnoid mater Pia mater Subarachnoid space Central canal (cerebrospinal fluid) Spinal meninges Spinal cord Subarachnoid space of spinal cord Structure and Function of the Nervous System • Meningitis: inf mm f la ation of the meninges • Encephalitis: inflammation of the brain • Meningoencephalitis: inflammation of both Bacterial Diseases of the Nervous System Learning Objectives Discuss the epidemiology of meningitis caused by Haemophilus influenzae, Neisseria meningitidis, Streptococcus pneumoniae, and Listeria monocytogenes. Explain how bacterial meningitis is diagnosed and treated. Learning Objectives Discuss the epidemiology of tetanus, Bacterial Diseases of the Nervous System p gy including mode of transmission, etiology, disease symptoms, and preventive measures. State the causative agent, symptoms, suspect f d d t t t f t foods, and treatment for botulism
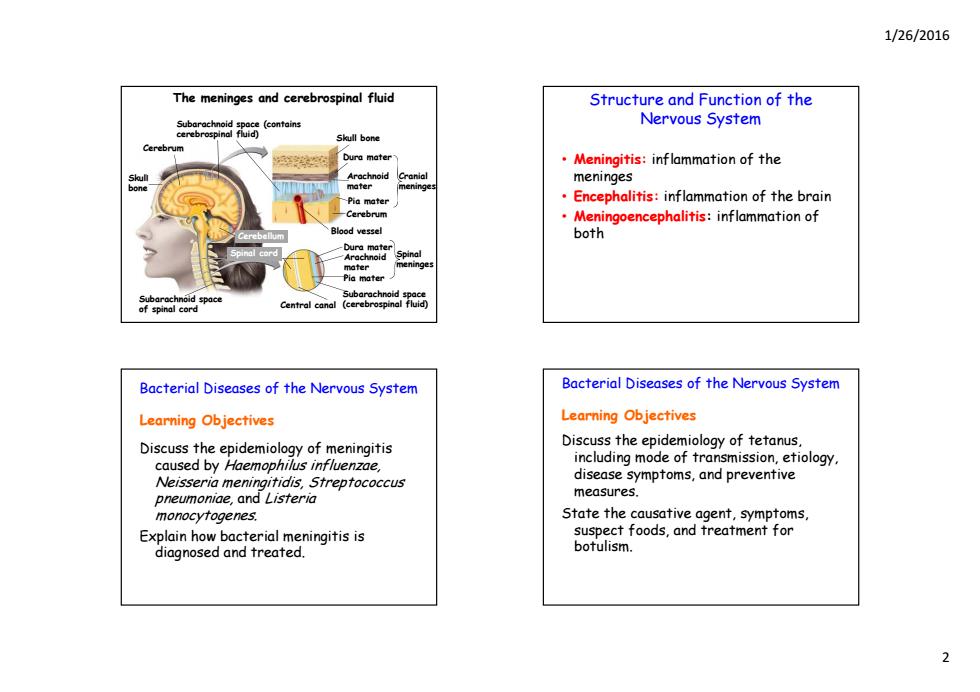
1/26/2016 Bacterial Meningitis toms of fever,headache,and Normal meninges Followed by nausea and vomiting May progress to convulsions and coma Death from shock and inflammation Due to endotoxin and cell wall release Three main bacterial species Meningitis Haemophilus influenza Neisseria meningitidis Streptococcus pneumoniae 50 other opportunistic bacterial species Listeria monocytogenes Haemophilus influenzae Meningitis Neisseria meningitidis Meningitis (Meningococcal Meningitis) Gram-negative aerobic cocci with a capsule Gram-negative aerobic bacteria -Six serotypes associated with the disease a。 Normal throat microbiota 4%f people are healthy nasopharyngeal Can enter the bloodstream carriers Pathogenicity due to capsule antigen type b Begins as a throat infection,rash,and bacteremia Occurs mostly in children(6 months to 4 yrs) Endotoxin leads to meningitis and death quickly Prevented by the Hib vaccine Mortality of 9-12%with antibiotic therapy:80% without Accounts for 45%of bacterial meningitis cases:6%mortality Outbreaks common in dorms and military barracks Vaccination protects against some serotypes
1/26/2016 3 Bacterial Meningitis • Initial symptoms of fever, headache, and a stiff neck • Followed by nausea and vomiting • May progress to convulsions and coma • Death from shock and inflammation – Due to endotoxin and cell wall release • Three main bacterial species Haemophilus influenza Neisseria meningitidis Streptococcus pneumoniae • 50 other opportunistic bacterial species Listeria monocytogenes Haemophilus influenzae Meningitis • Gram-negative aerobic bacteria • N l h i bi Normal throat microbiota • Can enter the bloodstream • Pathogenicity due to capsule antigen type b • Occurs mostly in children (6 months to 4 yrs) • Prevented by the Hib vaccine • Accounts for 45% of bacterial meningitis cases; 6% mortality Neisseria meningitidis Meningitis (Meningococcal Meningitis) • Gram-negative aerobic cocci with a capsule – Six serotypes associated with the disease • 40% of people are healthy nasopharyngeal carriers • Begins as a throat infection, rash, and bacteremia • Endotoxin leads to meningitis and death quickly • Mortality of 9–12% with antibiotic therapy; 80% without • Outbreaks common in dorms and military barracks • Vaccination protects against some serotypes
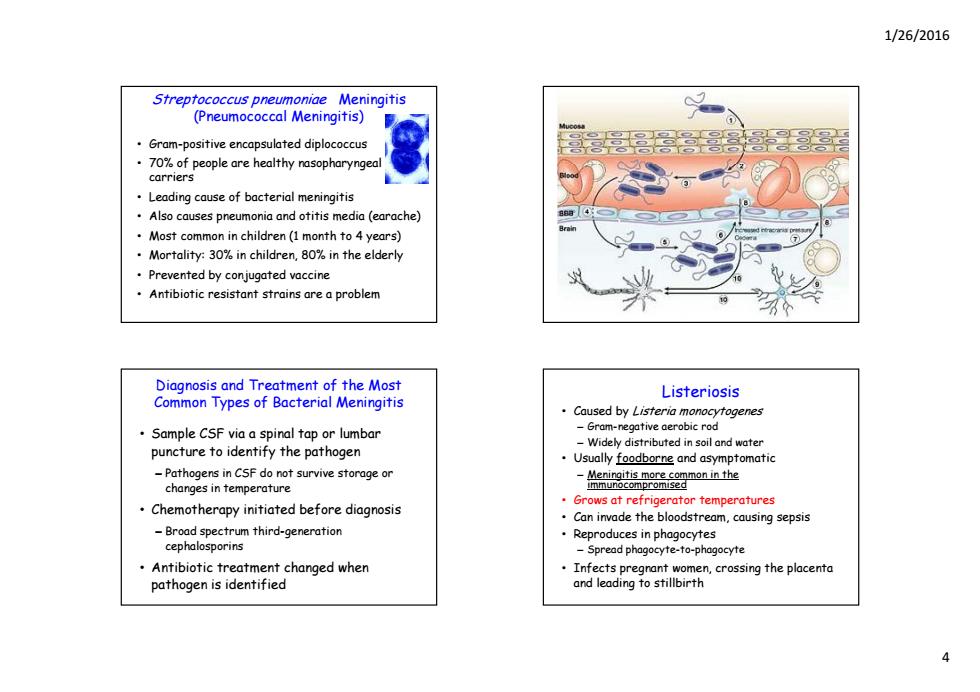
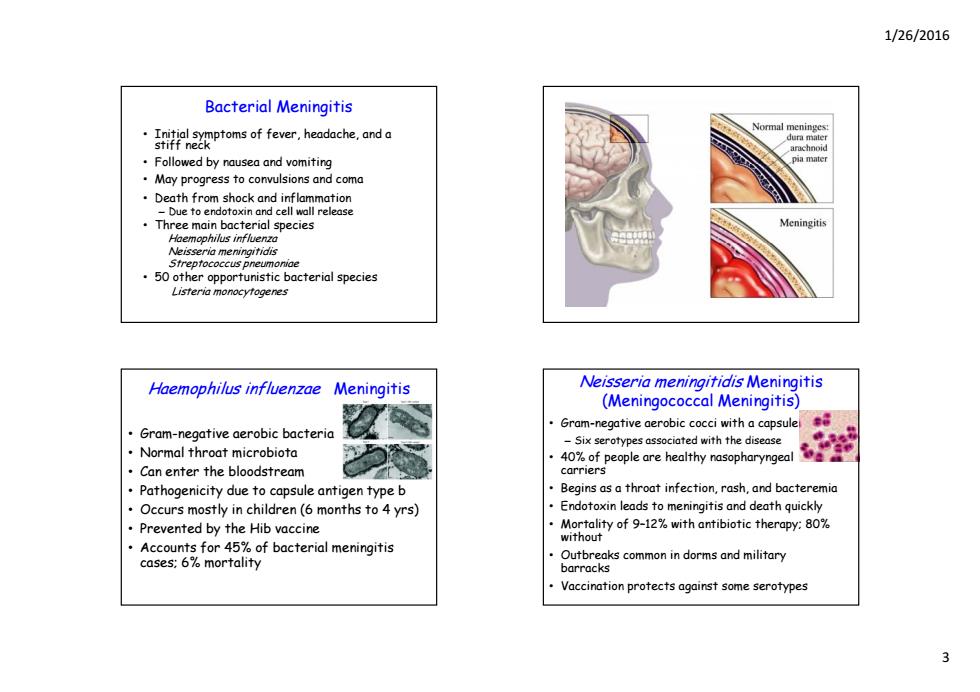
1/26/2016 Streptococcus pneumoniae Meningitis (Pneumococcal Meningitis) Gram-positive encapsulated diplococcus .70%of people are healthy nasopharyngeal carriers Leading cause of bacterial meningitis Also causes pneumonia and otitis media (earache) Most common in children(1 month to 4 years) Mortality:30%in children,80%in the elderly Prevented by conjugated vaccine Antibiotic resistant strains are a problem Diagnosis and Treatment of the Most Listeriosis Common Types of Bacterial Meningitis Caused by Listeria monocytogenes Sample CSF via a spinal tap or lumbar -Gram-negative aerobic rod -Widely distributed in soil and water puncture to identify the pathogen Usually foodborne and asymptomatic -Pathogens in CSF do not survive storage or changes in temperature .Chemotherapy initiated before diagnosis Grows at refrigerator temperatures Can invade the bloodstream,causing sepsis -Broad spectrum third-generation Reproduces in phagocytes cephalosporins -Spread phagocyte-to-phagocyte Antibiotic treatment changed when Infects pregrant women,crossing the placenta pathogen is identified and leading to stillbirth
1/26/2016 4 Streptococcus pneumoniae Meningitis (Pneumococcal Meningitis) • Gram-positive encapsulated diplococcus • 70% of people are healthy nasopharyngeal carriers • Leading cause of bacterial meningitis • Also causes pneumonia and otitis media (earache) • Most common in children (1 month to 4 years) • Mortality: 30% in children, 80% in the elderly • Prevented by conjugated vaccine • Antibiotic resistant strains are a problem Diagnosis and Treatment of the Most Common Types of Bacterial Meningitis • Sample CSF via a spinal tap or lumbar punct t id tif th th ture to identify the pathogen – Pathogens in CSF do not survive storage or changes in temperature • Chemotherapy initiated before diagnosis – B d hi d Broad spectrum third-generati on cephalosporins • Antibiotic treatment changed when pathogen is identified Listeriosis • Caused by Listeria monocytogenes – Gram-negative aerobic rod – Widely distributed in soil and water • Usually foodborne and asymptomatic – Meningitis more common in the immunocompromised • Grows at refrigerator temperatures • Can invade the bloodstream, causing sepsis • Reproduces in phagocytes – Spread phagocyte-to-phagocyte • Infects pregnant women, crossing the placenta and leading to stillbirth
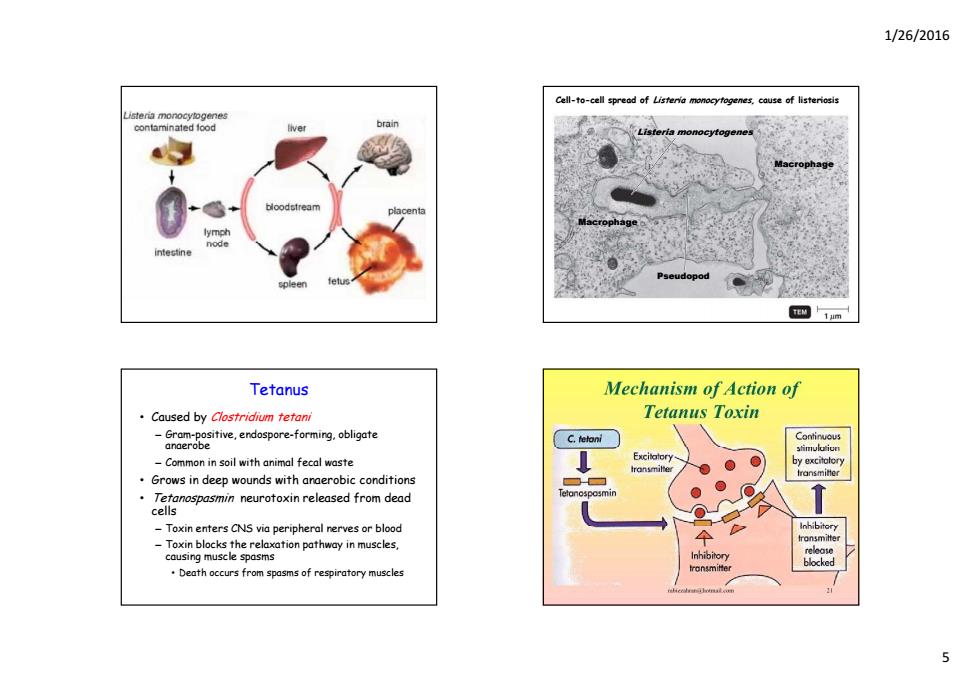
1/26/2016 Cell-to-cell spread of Listeria monoeyfogenes,cause of listeriosis contaminated food ve brain isteria monocytogenes Pseudopod M1am Tetanus Mechanism of Action of Caused by Clostridium tetani Tetanus Toxin ore-frgote Continuous stimuloion -Common in soil with animal fecal waste by excitolery Grows in deep wounds with anaerobic conditions -Toxin enters CNS via peripheral nerves or blood Inhibitory -Toxin blocks the relaxation pathway in muscles, fransmiter causing muscle spasms Inhibitory transmitter blocked Death occurs from spasms of respiratory muscles
1/26/2016 5 Cell-to-cell spread of Listeria monocytogenes, cause of listeriosis Listeria monocytogenes Macrophage Macrophage Pseudopod Tetanus • Caused by Clostridium tetani – Gram-positive, endospore-forming, obligate anaerobe – Common in soil with animal fecal waste • Grows in deep wounds with anaerobic conditions • Tetanospasmin neurotoxin released from dead cells – Toxin enters CNS via peripheral nerves or blood – Toxin blocks the relaxation pathway in muscles, causing muscle spasms • Death occurs from spasms of respiratory muscles
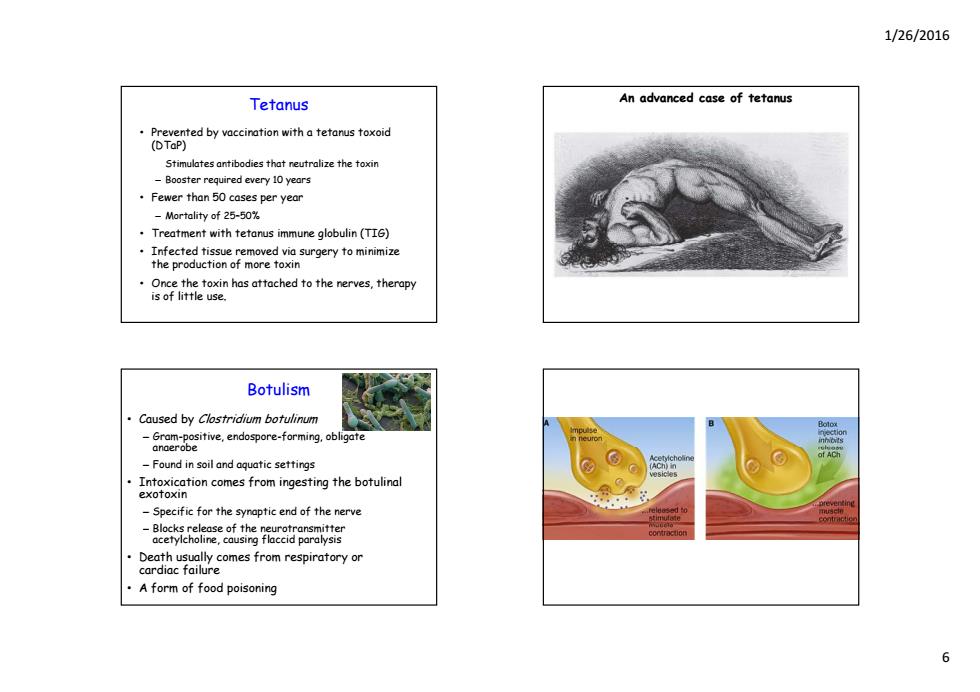
1/26/2016 Tetanus An advanced case of tetanus Prevented by vaccination with a tetanus toxoid (DTaP) Stimulates antibodies that neutralize the toxin -Booster required every 10 years Fewer than 50 cases per year Mortality of 25-50% Treatment with tetanus immune globulin (TIG) Infected tissue removed via surgery to minimize the production of more toxin Botulism Caused by Clostridium botulinum -Gram-positive,endospore-forming,obligate anderobe -Found in soil and aquatic settings Intoxication comes from ingesting the botulinal exoToxIn -Specific for the synaptic end of the nerve Death usually comes from respiratory or cardiac failure A form of food poisoning 6
1/26/2016 6 Tetanus • Prevented by vaccination with a tetanus toxoid (DTaP) – Stimulates antibodies that neutralize the toxin – Booster required every 10 years • Fewer than 50 cases per year – Mortality of 25–50% • Treatment with tetanus immune globulin (TIG) • Infected tissue removed via surgery to minimize the production of more toxin • Once the toxin has attached to the nerves, therapy is of little use. An advanced case of tetanus Botulism • Caused by Clostridium botulinum – Gram-positive, endospore-forming, obligate anaerobe – Found in soil and aquatic settings • Intoxication comes from ingesting the botulinal exotoxin – Specific for the synaptic end of the nerve – Bl cks l s f th n u t nsmitt Blocks release of the neurotransmitter acetylcholine, causing flaccid paralysis • Death usually comes from respiratory or cardiac failure • A form of food poisoning

1/26/2016 Botulinal Types Incidence and Treatment of Botulism ·Type A toxin Infant botulism:C.botulinum growing in -Fatality:60-70%.food was only tasted,not swallowed the intestines of infants due to a lack of -Heat-resistant and proteolytic intestinal microbiota Type B toxin -Associated with honey -Fatality:25% .Wound botulism:growth of C.botulinum in ·Type E toxin wounds -Produced by organisms in marine and lake sediments Treatment with respiratory assistance and -Less heat-resistant than other strains antitoxins Diagnosed by inoculating immunized mice with Prevented with proper canning and the use patient samples of nitrites in foods Viral Diseases of the Nervous Poliomyelitis System Caused by the poliovirus Learning Objectives Transmitted by the ingestion of water containing feces containing the virus Discuss the epidemiology of poliomyelitis and Initial symptoms:sore throat and nausea rabies,including mode of transmission, etiology,and disease symptoms. Viremia may occur:enters the CNS -One percent of cases become paralytic Compare the Salk and Sabin polio vaccines. -Destruction of motor cells Compare the preexposure and postexposure -Virus replicates in the motor nerve cells leading to cell death treatments for rabies. -Death from respiratory failure Postpolio syndrome:muscle weakness occurring decades after infection
1/26/2016 7 Botulinal Types • Type A toxin – Fatality: 60–70%, food was only tasted, not swallowed – H t ea -resi t t d t l ti istant and proteolytic • Type B toxin – Fatality: 25% • Type E toxin – Produced by organisms in marine and lake sediments – Less heat-resistant than other strains • Diagnosed by inoculating immunized mice with patient samples Incidence and Treatment of Botulism • Infant botulism: C. botulinum growing in the intestines of infants due to a lack of intestinal microbiota – Associated with honey • Wound botulism: growth of C. botulinum in wounds • Treatment w reatment w th resp ratory ass stance and ith respiratory assistance and antitoxins • Prevented with proper canning and the use of nitrites in foods Viral Diseases of the Nervous System Learning Objectives Discuss the epidemiology of poliomyelitis and rabies, including mode of transmission, etiology, and disease symptoms. Compare the Salk and Sabin polio vaccines. Compare the preexposure and postexposure treatments for rabies. Poliomyelitis • Caused by the poliovirus • Transmitted by the ingestion of water containing feces containing the virus • Initial symptoms: sore throat and nausea • Viremia may occur; enters the CNS – One percent of cases become paralytic – Destruction of motor cells – Virus replicates in the motor nerve cells leading to cell death – Death from respiratory failure • Postpolio syndrome: muscle weakness occurring decades after infection
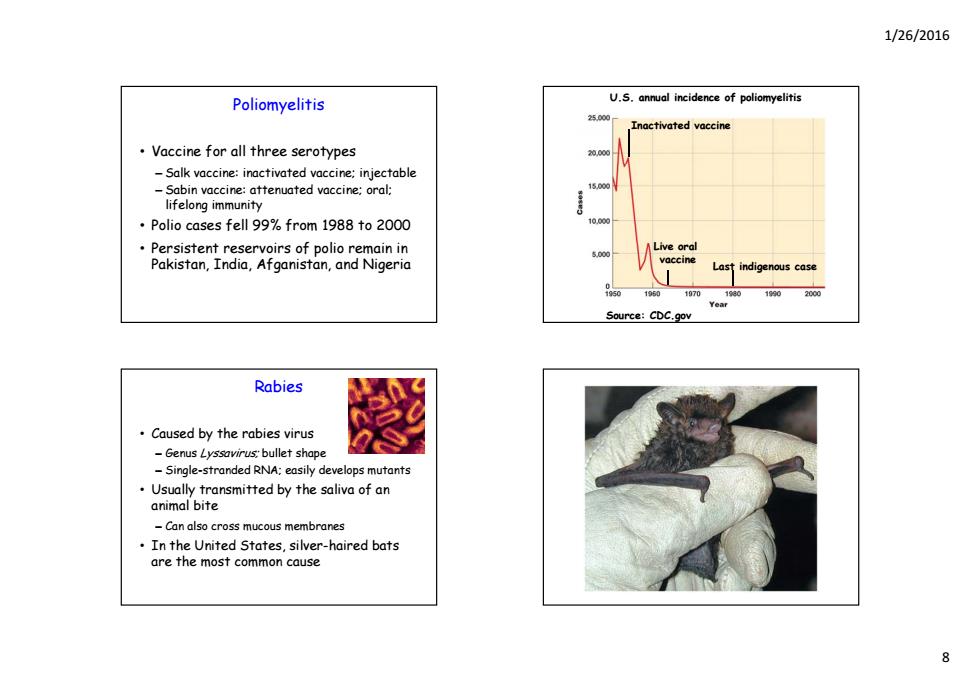
1/26/2016 Poliomyelitis U.S.annual incidence of poliomyelitis Inactivated vaccine Vaccine for all three serotypes -Salk vaccine:inactivated vaccine:injectable -Sabin vaccine:attenuated vaccine:oral: lifelong immunity Polio cases fell 99%from 1988 to 2000 Persistent reservoirs of polio remain in Pakistan,India,Afganistan,and Nigeria indigenous case 0 1060107019301990200 Year Source:CDC.gov Rabies Caused by the rabies virus Genus Lyssavirus:bullet shape -Single-stranded RNA:easily develops mutants Usually transmitted by the saliva of an animal bite -Can also cross mucous membranes In the United States,silver-haired bats are the most common cause
1/26/2016 8 Poliomyelitis • Vaccine for all three serotypes – Salk vaccine: inactivated vaccine; injectable – Sabin vaccine: attenuated vaccine; oral; lifelong immunity • Polio cases fell 99% from 1988 to 2000 • P i t t i f li i i Persistent reservoirs of polio remain in Pakistan, India, Afganistan, and Nigeria U.S. annual incidence of poliomyelitis Inactivated vaccine Li lve ora vaccine Last indigenous case Source: CDC.gov Rabies • Caused by the rabies virus – Genus Lyssavirus; bullet shape – Single-stranded RNA; easily develops mutants • Usually transmitted by the saliva of an animal bite – Can also cross mucous membranes • In the United States, silver-haired bats are the most common cause

1/26/2016 Rabies Pathology of rabies infection Initial symptoms:muscle spasms of the mouth and pharynx:hydrophobia encephalitis -Average incubation of 30 to 50 days Furious (classical)rabies:animals are restless,ther highly excitable Paralytic (dumb or numb)rabies:animals seem unaware of their surroundings:minimally excitable Rabies Rabies Diagnosed from bodily fluids with ·Global distribution the direct fluorescent-antibody (DFA)test In the United States,it occurs in bats Postexposure prophylaxis (PEP) skunks,foxes,raccoons,and domestic vaccine plus immune globulin animals H diploid cell vaccine (HDCV) Negative DFA test -Rarely in squirrels,rabbits,rats,and mice abies immune globulin (RIG) 7000 to 8000 animal cases of rabies in the United States annually Very little effective treatment the One to six human cases in the United reported States annually
1/26/2016 9 Rabies • Initial symptoms: muscle spasms of the mouth and pharynx; hydrophobia • Virus multiplies in the skeletal muscles and travels through the PNS to the brain cells, causing encephalitis – Average incubation of 30 to 50 days – Post exposure vaccination will work due to long incubation time • Furious (classical) rabies: animals are restless, then highly excitable • Paralytic (dumb or numb) rabies: animals seem unaware of their surroundings; minimally excitable Pathology of rabies infection Rabies • Diagnosed from bodily fluids with the direct fluorescent-antibody (DFA) test Positive DFA test ( ) • Postexposure prophylaxis (PEP): vaccine plus immune globulin – Human diploid cell vaccine (HDCV) – Human rabies immune globulin (RIG) Negative DFA test • Very little effective treatment once the symptoms appear and only a handful of survivors are reported Rabies • Global distribution • In the Un In the Un ted States, t occurs n bats, ited States, it occurs in bats, skunks, foxes, raccoons, and domestic animals – Rarely in squirrels, rabbits, rats, and mice • 7000 to 8000 animal cases of rabies in the United States annually • One to six human cases in the United States annually
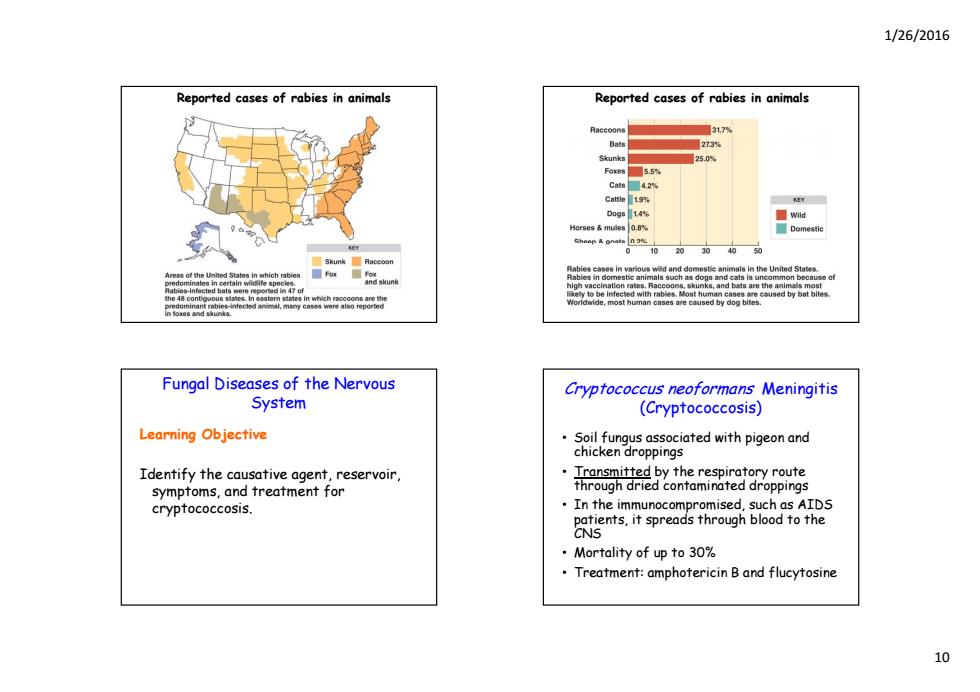
1/26/2016 Reported cases of rabies in animals Reported cases of rabies in animals 31,7 Bats 273% 25.0 Foxes5.5% Cats 4.2% D09s14 ■Wd Horses mules 0.8% Domestic 01020304050 是Skunk Racoon d ba nGega t h Fungal Diseases of the Nervous Cryptococcus neoformans Meningitis System (Cryptococcosis) Learning Objective Soil fungus associated with pigeon and chicken droppings Identify the causative agent,reservoir, Transmitted by the respiratory route symptoms,and treatment for through dried contaminated droppings crypfococcosis. In the immunocompromised,such as AIDS patients,it spreads through blood to the CNS ·Mortality of up to30% Treatment:amphotericin B and flucytosine 10
1/26/2016 10 Reported cases of rabies in animals Reported cases of rabies in animals Fungal Diseases of the Nervous System Learning Objective Identify the causative agent, reservoir, symptoms, and treatment for cryptococcosis. Cryptococcus neoformans Meningitis (Cryptococcosis) • Soil fungus associated with pigeon and chi k d i hicken droppings • Transmitted by the respiratory route through dried contaminated droppings • In the immunocompromised, such as AIDS ppg atients, it spreads through blood to the CNS • Mortality of up to 30% • Treatment: amphotericin B and flucytosine