Week 12 Quiz 4 Cardiac pathology Elsevier 2005 1.A 68 year old man with a history of diabetes mellitus had chest pain and an elevated serum troponin I level year ago.He was treated in the hospital with anti-arrhythmic agents for 1 week.An echocardiogram showed an ejection fraction of 28%.He now has markedly reduced exercise tolerance.On physical examination his temperature is 37C,pulse 68/min,respirations 176/min,and blood pressure 130/80 mm Hg.Diffuse crackles are heard on auscultation of the lungs.The representative cross appearance of the heart is shown in the preceding figure.Which of the following complications of this disease is the patient MOST LIKELY to develop? A Atrial myxoma B.Cardiac tamponade C Constricti ericarditis D.Hypertrophi E.System thromboe Ans:E This enlarged and dilated heart has a large venricular anewrysm.The aneurysm most likely resulted from lar wall at the site ofa prior healed myocardial infarction (MI).Because of the damage to the endocardial linint stasis and urbulence of ld o in the region of the aneuysm.mral thrombi are likely to develop.When detached.these thrombi embolize to the systemic circulation and can cause infarcts elsewhere.An atrial myxoma is the most common primary cardiac neoplasm,but it is rare and it is not related to ischemic heart disease.Cardiac rupture with tamponade is most likely to occur 5 to 7 days after an acute MI.Constrictive pericarditis follows a previous suppurative or tuberculous pericarditis.Hypertrophic cardiomyopathy is not related to ischemic heart disease,but 50%of cases are familial and may be related to mutations in genes encoding cardiac contractile elements. 2.A 50 year old man has sudden onset of severe substernal chest pain that radiates to the neck.On physical examination he is afebrile but has tachycardia.hyperventilation,and hyp otension no cardiac murmurs are heard on auscultation.Emergent coronary an raphy shows a thrombotic occ lusion of the left circumflex artery and areas of 50%to 70%na wing in the imal circumflex and anterior descending arteries Which A.Constricti
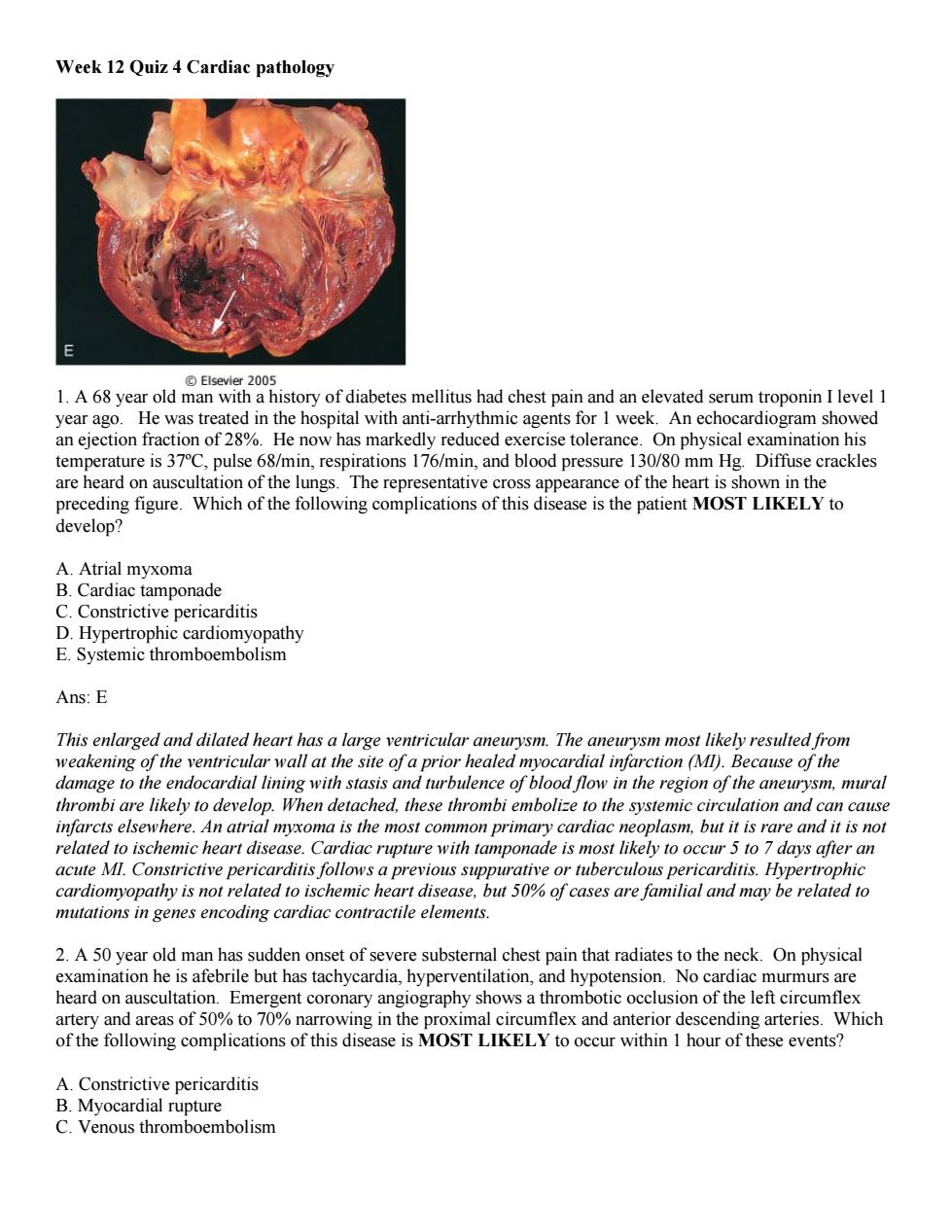
Week 12 Quiz 4 Cardiac pathology 1. A 68 year old man with a history of diabetes mellitus had chest pain and an elevated serum troponin I level 1 year ago. He was treated in the hospital with anti-arrhythmic agents for 1 week. An echocardiogram showed an ejection fraction of 28%. He now has markedly reduced exercise tolerance. On physical examination his temperature is 37ºC, pulse 68/min, respirations 176/min, and blood pressure 130/80 mm Hg. Diffuse crackles are heard on auscultation of the lungs. The representative cross appearance of the heart is shown in the preceding figure. Which of the following complications of this disease is the patient MOST LIKELY to develop? A. Atrial myxoma B. Cardiac tamponade C. Constrictive pericarditis D. Hypertrophic cardiomyopathy E. Systemic thromboembolism Ans: E This enlarged and dilated heart has a large ventricular aneurysm. The aneurysm most likely resulted from weakening of the ventricular wall at the site of a prior healed myocardial infarction (MI). Because of the damage to the endocardial lining with stasis and turbulence of blood flow in the region of the aneurysm, mural thrombi are likely to develop. When detached, these thrombi embolize to the systemic circulation and can cause infarcts elsewhere. An atrial myxoma is the most common primary cardiac neoplasm, but it is rare and it is not related to ischemic heart disease. Cardiac rupture with tamponade is most likely to occur 5 to 7 days after an acute MI. Constrictive pericarditis follows a previous suppurative or tuberculous pericarditis. Hypertrophic cardiomyopathy is not related to ischemic heart disease, but 50% of cases are familial and may be related to mutations in genes encoding cardiac contractile elements. 2. A 50 year old man has sudden onset of severe substernal chest pain that radiates to the neck. On physical examination he is afebrile but has tachycardia, hyperventilation, and hypotension. No cardiac murmurs are heard on auscultation. Emergent coronary angiography shows a thrombotic occlusion of the left circumflex artery and areas of 50% to 70% narrowing in the proximal circumflex and anterior descending arteries. Which of the following complications of this disease is MOST LIKELY to occur within 1 hour of these events? A. Constrictive pericarditis B. Myocardial rupture C. Venous thromboembolism
Ans:E In the period immediately following coronary thrombosis.arrhythmias are the most important complication and can lead to sudden cardiac death.It is believed that,even before ischemic injury manifests in the heart,there is greatly increased electrical irritability.Constrictive pericarditis and myocardial rupture occur several days later.Ifportions of a coronary thrombus break off and embolize,they enter smaller arterial branches in the vascular distribution which is already affected by ischemia and thus cause no further injury.Ventricular aneurysm is a late complication of healing of a large transmural infarction.A mural thrombus may fill an aneurysm and become a source of emboli. 3.A59-year-old man has experienced chronic fatigue for the past 18 months.On physical examination he is afebrile.A chest radiograph shows bilateral pulmonary edema and a prominent border on the left side of the heart.The representative gross appearance of the heart is shown.Laboratory studies show serum glucose of 74 mg/dL,total cholesterol 189 mg/dL,total protein 7.1 g/dL,albumin 5.2 g/dL,creatinine 6.1 mg/dL,and urea nitrogen 58 mg/dL.Which of the following is the MOST LIKELY diagnosis? A.Chronic alcoholism B.Diabetes mellitus C.Hemochromatosis D.Pneumoconiosis E.Sy stemic hypertension Ans:E with ch onic ren e. etes mellitus lerates atherosclerosis,lead ing to ischemic heart disease and myocardial infarction.Hemachromatosis leads to restrictive cardiomyopathy.Pneumonconioses produce restrictive lung disease with corpulmonale and predominantly right ventricular hypertrophy. 4.A 60 year old man has experienced angina on exertion for the past 6 years.A coronary angiogram performed 2 years ago showed 75%stenosis of the left anterior descending coronary artery and 50%stenosis of the right coronary artery.For the past 3 weeks the frequency and severity of the anginal attacks have increased and pain sometimes occurs even when he is lying in bed.On physical examination his blood pressure is 110/80 mm Hg and pulse is 85/min with irregular beats.Laboratory studies show serum glucose of 188 mg/dL,creatinine 1.2 mg/dL,and troponin I 1.5 ng/mL.Which of the following is MOST LIKELY to explain these findings?
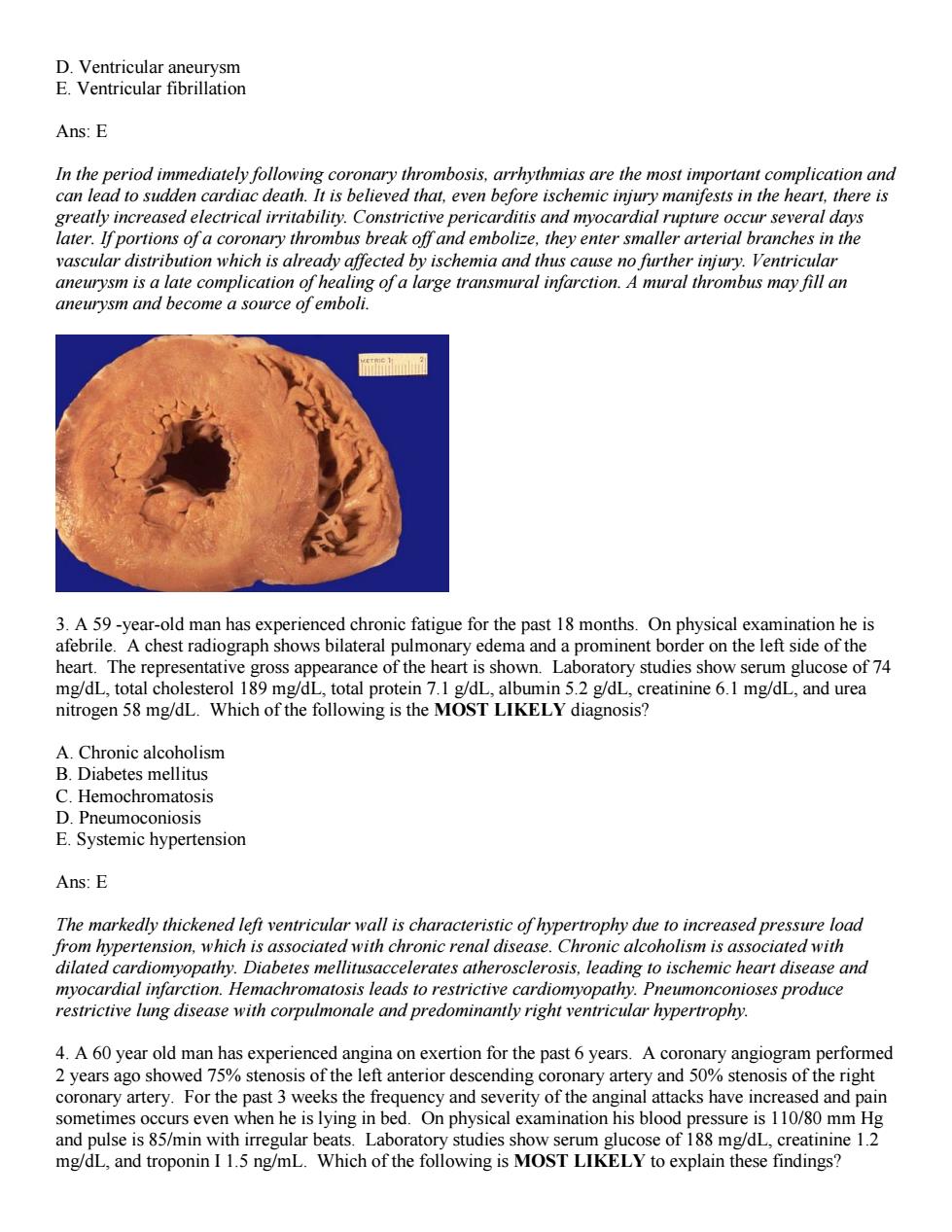
D. Ventricular aneurysm E. Ventricular fibrillation Ans: E In the period immediately following coronary thrombosis, arrhythmias are the most important complication and can lead to sudden cardiac death. It is believed that, even before ischemic injury manifests in the heart, there is greatly increased electrical irritability. Constrictive pericarditis and myocardial rupture occur several days later. If portions of a coronary thrombus break off and embolize, they enter smaller arterial branches in the vascular distribution which is already affected by ischemia and thus cause no further injury. Ventricular aneurysm is a late complication of healing of a large transmural infarction. A mural thrombus may fill an aneurysm and become a source of emboli. 3. A 59 -year-old man has experienced chronic fatigue for the past 18 months. On physical examination he is afebrile. A chest radiograph shows bilateral pulmonary edema and a prominent border on the left side of the heart. The representative gross appearance of the heart is shown. Laboratory studies show serum glucose of 74 mg/dL, total cholesterol 189 mg/dL, total protein 7.1 g/dL, albumin 5.2 g/dL, creatinine 6.1 mg/dL, and urea nitrogen 58 mg/dL. Which of the following is the MOST LIKELY diagnosis? A. Chronic alcoholism B. Diabetes mellitus C. Hemochromatosis D. Pneumoconiosis E. Systemic hypertension Ans: E The markedly thickened left ventricular wall is characteristic of hypertrophy due to increased pressure load from hypertension, which is associated with chronic renal disease. Chronic alcoholism is associated with dilated cardiomyopathy. Diabetes mellitusaccelerates atherosclerosis, leading to ischemic heart disease and myocardial infarction. Hemachromatosis leads to restrictive cardiomyopathy. Pneumonconioses produce restrictive lung disease with corpulmonale and predominantly right ventricular hypertrophy. 4. A 60 year old man has experienced angina on exertion for the past 6 years. A coronary angiogram performed 2 years ago showed 75% stenosis of the left anterior descending coronary artery and 50% stenosis of the right coronary artery. For the past 3 weeks the frequency and severity of the anginal attacks have increased and pain sometimes occurs even when he is lying in bed. On physical examination his blood pressure is 110/80 mm Hg and pulse is 85/min with irregular beats. Laboratory studies show serum glucose of 188 mg/dL, creatinine 1.2 mg/dL, and troponin I 1.5 ng/mL. Which of the following is MOST LIKELY to explain these findings?

Hypertrophy of chemc myocardium with inereased(atial)thrombus B.Hypertrophy oxygen deman corona D Re ea ry arte rying capacity du le to pulmonary congestion Ans:A This patient has 75%stenosis of the left anterior descending branch of the coronary artery.This degree of stenosis prevents adequate perfusion of the heart when myocardial demand is increased.which occurs during exertion.Hence the patient has angina on exertion.The patient has recently developed unstable angina,which is manifest by increased frequency and severity of attacks and angina at rest.In most patients,unstable angina is produced by disruption of an atherosclerotic plaque followed by mural thrombus and possibly distal embolization,vasospasm or both.Hypertrophy of the heart is unlikely in this case,because there is neither hypertension nor a valvular lesion.Increased stenosis of the right coronary artery,pulmonary congestion or complete occlusion of both coronary arteries can theoretically give rise to a similar clinical picture,but plaque disruption with mural thrombus is the most common anatomic finding when a patient develops unstable angina. Unstable angina is a harbinger of myocardial infarction
A. Erosion of plaque in left coronary artery with superimposed mural (partial) thrombus B. Hypertrophy of ischemic myocardium with increased oxygen demands C. Increasing stenosis of right coronary artery D. Reduction in oxygen-carrying capacity due to pulmonary congestion E. Sudden, complete thrombotic occlusion of right and left coronary arteries Ans: A This patient has 75% stenosis of the left anterior descending branch of the coronary artery. This degree of stenosis prevents adequate perfusion of the heart when myocardial demand is increased, which occurs during exertion. Hence the patient has angina on exertion. The patient has recently developed unstable angina, which is manifest by increased frequency and severity of attacks and angina at rest. In most patients, unstable angina is produced by disruption of an atherosclerotic plaque followed by mural thrombus and possibly distal embolization, vasospasm or both. Hypertrophy of the heart is unlikely in this case, because there is neither hypertension nor a valvular lesion. Increased stenosis of the right coronary artery, pulmonary congestion or complete occlusion of both coronary arteries can theoretically give rise to a similar clinical picture, but plaque disruption with mural thrombus is the most common anatomic finding when a patient develops unstable angina. Unstable angina is a harbinger of myocardial infarction
於t油 ocardial infarction was documented at autopsy The gross and with the degree of coronary atherosclerosi and its complicatio ,clinical symptoms,an therapies given before deat morrhage and contraction bands in necrotic myocardial fibers are MOST LIKELY to be seen in which of the following types of infarcts? A.Healing transmural myocardial infarct B.Subendocardial infarct resulting from diffuse narrowing or coronary arteries C.Transmural infarct caused by complete thrombotic occlusion of a coronary artery D.Transmural infarct complicated by mural thrombosis E.Transmural infarct reperfused by thrombolytic therapy AnsF Reperfusion of an ischemic mvocardium by spontaneous or therapeutic thrombolysis changes the morphologic features of the affected a period of ischemia leads to of blood into the rhage).Co ction bands f closely acked ted are m likely pro sly injured are exposed to a high the aThe membran be a prominent feature of the other options 6.Which procedure yields the HIGHEST incidence of vessel patency after 10 years? A.Aspirin plus Plavix,p.o. B.Balloon angioplasty,left anterior descending coronary artery C.Bare endoluminal stent in left anterior descending coronary artery D.Left internal thoracic(mammary)artery to left anterior descending coronary artery E.Reverse saphenous vein to left anterior descending coronary artery Ans:D Clinical trials have demonstrated that arterial grafting to circumvent a region of stenosis maintains the highest incidence of vessel patency over the long term.As pirin and Plavix minimize the risk of thrombotic occlusion of an artery narrowed by atherosclerotic plac ue.Ballo gioplasty is an effective immediate therapy,but dueto eated vessel y bec over the longtermA bare sten may be thro
5. A study of ischemic heart disease analyzes cases in which myocardial infarction was documented at autopsy. The gross and microscopic appearances of the hearts are correlated with the degree of coronary atherosclerosis and its complications, clinical symptoms, and therapies given before death. Hemorrhage and contraction bands in necrotic myocardial fibers are MOST LIKELY to be seen in which of the following types of infarcts? A. Healing transmural myocardial infarct B. Subendocardial infarct resulting from diffuse narrowing or coronary arteries C. Transmural infarct caused by complete thrombotic occlusion of a coronary artery D. Transmural infarct complicated by mural thrombosis E. Transmural infarct reperfused by thrombolytic therapy Ans: E Reperfusion of an ischemic myocardium by spontaneous or therapeutic thrombolysis changes the morphologic features of the affected area. Reflow of blood into the vasculature injured during a period of ischemia leads to leakage of blood into the tissues (hemorrhage). Contraction bands are composed of closely packed hypercontracted sarcomeres. They are most likely produced by exaggerated contraction of previously injured myofibrils that are exposed to a high concentration of calcium ions from the plasma. The damaged cell membrane of the injured myocardial cells allows calcium to penetrate the cells rapidly. Hemorrhage would not be a prominent feature of the other options. 6. Which procedure yields the HIGHEST incidence of vessel patency after 10 years? A. Aspirin plus Plavix, p.o. B. Balloon angioplasty, left anterior descending coronary artery C. Bare endoluminal stent in left anterior descending coronary artery D. Left internal thoracic (mammary) artery to left anterior descending coronary artery E. Reverse saphenous vein to left anterior descending coronary artery Ans: D Clinical trials have demonstrated that arterial grafting to circumvent a region of stenosis maintains the highest incidence of vessel patency over the long term. Aspirin and Plavix minimize the risk of thrombotic occlusion of an artery narrowed by atherosclerotic plaque. Balloon angioplasty is an effective immediate therapy, but due to intimal injury incurred during therapy the treated vessel may become occluded over the long term. A bare stent may be thrombogenic. While useful, a venous graft is less likely to remain patent than an arterial graft
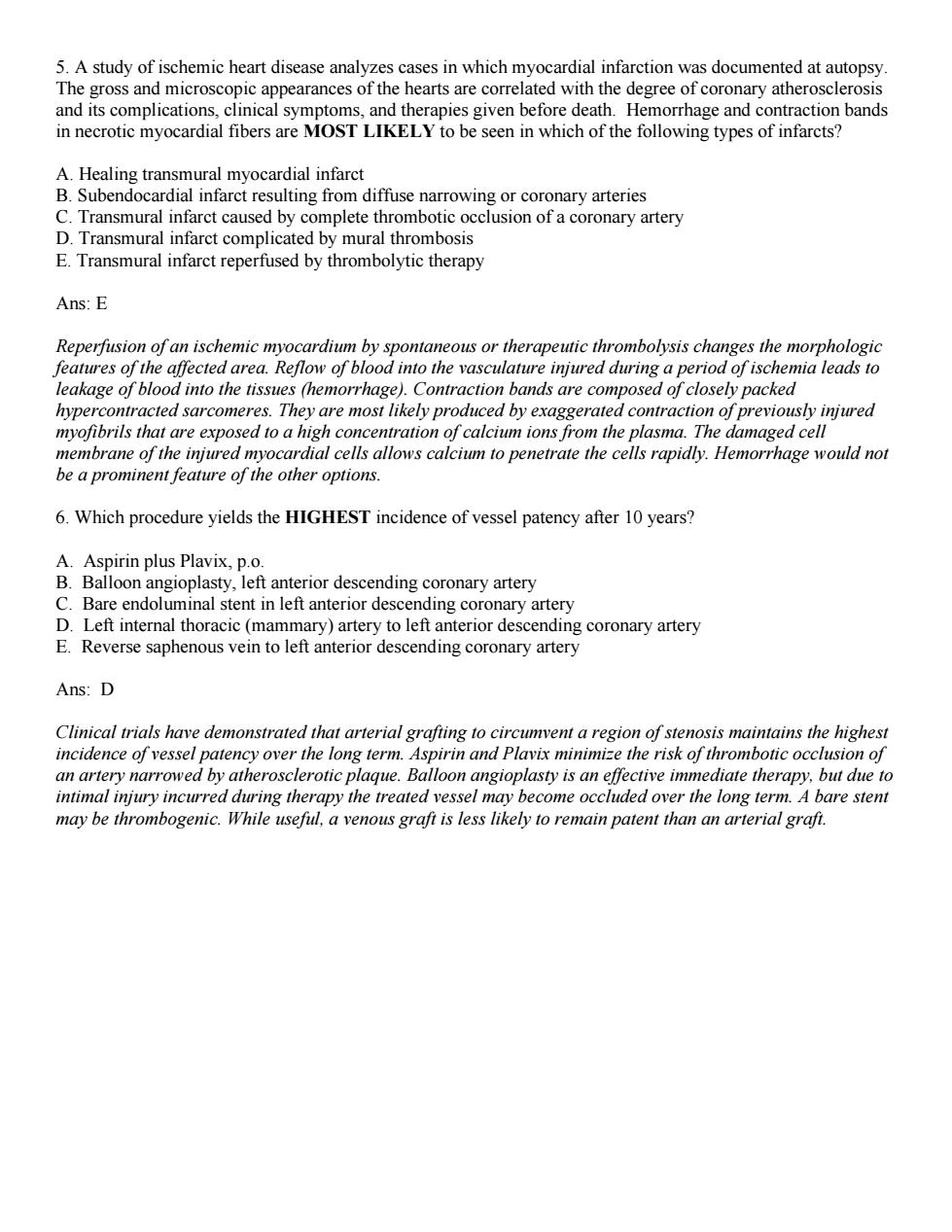
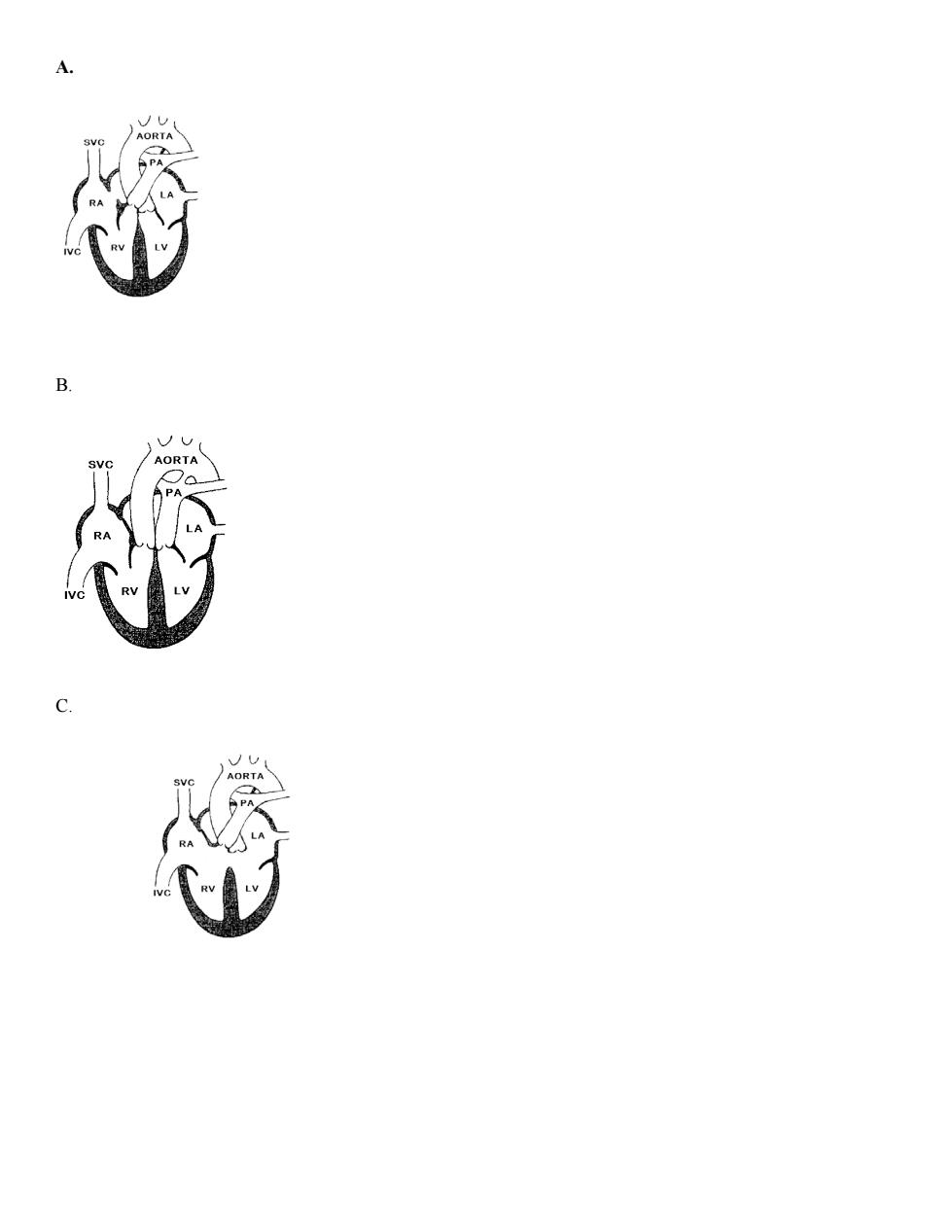
ORTA 7.A 4-year-old girl who is below the 5th percentile for height and weight for age becomes easily fatigued.On physical examination she appears cyanotic.Her temperature is 37C.pulse 82/min,respirations 16/min,and blood pressure 105/65 mm Hg.Arterial blood gas measurement shows decreased oxygen saturation.A diagram of the child's heart is shown above.Which of the following congenital heart diseases does she have? A.Atrial septal defect B.Coarctation of the aorta C.Patent ductus arteriosus D.Transposition of the great vessels E.Truncus arteriosus Ans:E Cyanosis at an early age suggests a right-to-lefi shunt.Truncus arteriosus,transposition of the great arteries and tetralogy of Fallot are the most common causes of cyanotic congenital heart disease.The figure shows a single great artery that receives blood from both ventricles.This featre is characteristic of persistent truncus arteriosus.Overriding aorta:ventricular septal defect:narrowing of the right ventricular ouflow tract and righ ventricular hypertrophy are features of tetralogy of Fallot.Transposition of the great arteries represents right ventricular ouflow to the aorta and left ventricular oufow to the pulmonary artery.Atrial septal defect and patent ductus arteriosus initially lead to lefi-to-right shunts.Coarctation is not accompanied by a shunt and cvanosis. 8.A 12-year-old boy complains of pain in his legs when he runs more than 300 meters.Physical examination shows temperature of 36.8C.pulse 76/min,respirations 22/min.and blood pressure 165/90mm Hg.The radia pulses are 4+,and the dorsalis pedis pulses are 1+.Arterial blood gas measurement shows a normal oxygen saturation level.Which of the following diagrams best illustrates his cardiac pathology?
7. A 4 -year-old girl who is below the 5th percentile for height and weight for age becomes easily fatigued. On physical examination she appears cyanotic. Her temperature is 37°C, pulse 82/min, respirations 16/min, and blood pressure 105/65 mm Hg. Arterial blood gas measurement shows decreased oxygen saturation. A diagram of the child's heart is shown above. Which of the following congenital heart diseases does she have? A. Atrial septal defect B. Coarctation of the aorta C. Patent ductus arteriosus D. Transposition of the great vessels E. Truncus arteriosus Ans: E Cyanosis at an early age suggests a right-to-left shunt. Truncus arteriosus, transposition of the great arteries and tetralogy of Fallot are the most common causes of cyanotic congenital heart disease. The figure shows a single great artery that receives blood from both ventricles. This feature is characteristic of persistent truncus arteriosus.Overriding aorta; ventricular septal defect; narrowing of the right ventricular outflow tract and right ventricular hypertrophy are features of tetralogy of Fallot. Transposition of the great arteries represents right ventricular outflow to the aorta and left ventricular outflow to the pulmonary artery. Atrial septal defect and patent ductus arteriosus initially lead to left-to-right shunts. Coarctation is not accompanied by a shunt and cyanosis. 8. A 12-year-old boy complains of pain in his legs when he runs more than 300 meters. Physical examination shows temperature of 36.8°C, pulse 76/min, respirations 22/min, and blood pressure 165/90 mm Hg. The radial pulses are 4+, and the dorsalis pedis pulses are 1+. Arterial blood gas measurement shows a normal oxygen saturation level. Which of the following diagrams best illustrates his cardiac pathology?
A
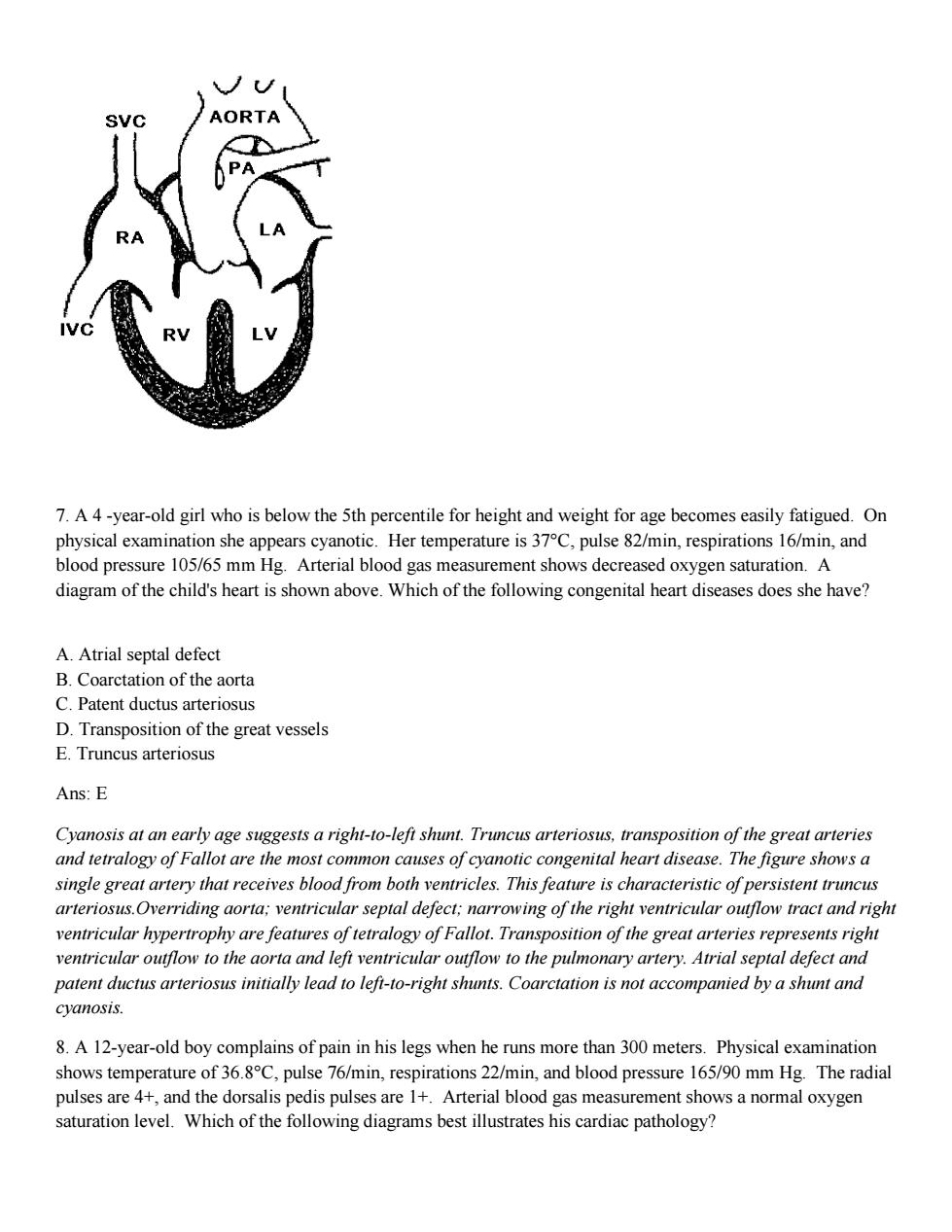
A. B. C
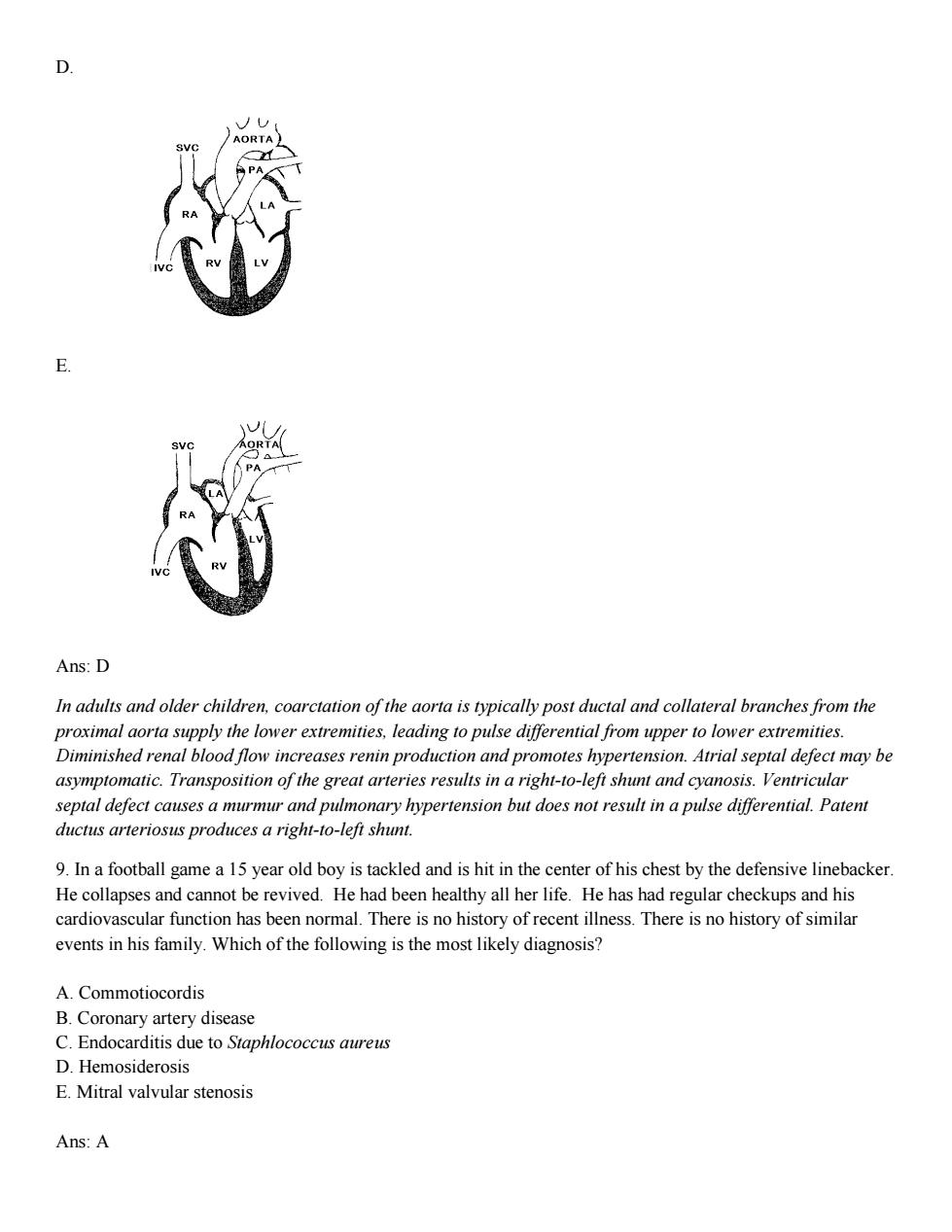
0 Ans:D In adults and older children.coarctation of the aorta is typically post ductal and collateral branches from the proximal aorta supply the lower extremities,leading to pulse differential from upper to lower extremities. Diminished renal blood flow increases renin production and promotes hypertension.Atrial septal defect may be asymptomatic.Transposition of the great arteries results in a right-to-left shunt and cyanosis.Ventricular septal defect causes a murmur and pulmonary hypertension but does not result in a pulse differential.Patent ductus arteriosus produces a right-to-left shunt. 9.In a football game a 15 year old boy is tackled and is hit in the center of his chest by the defensive linebacker. He collapses and cannot be revived.He had been healthy all her life.He has had regular checkups and his cardiovascular function has been normal.There is no history of recent illness.There is no history of simila events in his family.Which of the following is the most likely diagnosis? A.Commotiocordis B.Coronary artery disease C.Endocarditis due to Staphlococcus aureus D.Hemosiderosis E.Mitral valvular stenosis Ans:A
D. E. Ans: D In adults and older children, coarctation of the aorta is typically post ductal and collateral branches from the proximal aorta supply the lower extremities, leading to pulse differential from upper to lower extremities. Diminished renal blood flow increases renin production and promotes hypertension. Atrial septal defect may be asymptomatic. Transposition of the great arteries results in a right-to-left shunt and cyanosis. Ventricular septal defect causes a murmur and pulmonary hypertension but does not result in a pulse differential. Patent ductus arteriosus produces a right-to-left shunt. 9. In a football game a 15 year old boy is tackled and is hit in the center of his chest by the defensive linebacker. He collapses and cannot be revived. He had been healthy all her life. He has had regular checkups and his cardiovascular function has been normal. There is no history of recent illness. There is no history of similar events in his family. Which of the following is the most likely diagnosis? A. Commotiocordis B. Coronary artery disease C. Endocarditis due to Staphlococcus aureus D. Hemosiderosis E. Mitral valvular stenosis Ans: A
Commotiocordisis a lethal disruption of heart rhythm that occurs as a result ofa blow to the area directly over the heart at a critical time during the cycle ofa heart beat which results in ventricular fibrillation.Coronary artery disease resulting in inadequate myocardial perfusion is very rare at this age.Endocarditis presents with fever.chills and sweating.Hemosiderosis results from iron overload.Mitral valvular stenosis is a frequent complication of rheumatic heart disease.It presents clinically with signs and symptoms of heart failure such as dyspnea,orthopnea and paroxysmal nocturnal dyspnea. 10.A previously healthy 20 year old man develops heart failure over a period of several days.He is febrile and complains to his friends that he has chest pain,but he does not seek medical attention.He dies and an autopsy is performed.Examination of the heart shows that both ventricles are dilated but otherwise the myocardium appears normal by gross visual inspection.An H&E-stained histologic section shows numerous inflammatory cells in the myocard more than 80 individua round myocytes myocytes are necrotic. B.Acute myocardial C.Acute rheumatic fever D.Marantic endocarditis E.Viral myocarditis Ans:E Viral myocarditis ca heart failure use a mild disease without any symp opsy which sho eden mmatory es ver duals er or lymph ever is rare m mc uent popi rantlendocardn is ue ope vauon 11.A 31-year old woman has had increasing dyspnea for the past week.Physical examination shows temperature of 37.3C,pulse 85/min,respirations 20/min,and blood pressure 150/95 mm Hg.There is dullness to percussion over the lung bases.A chest radiograph shows large bilateral pleural effusions and a normal heart size.Laboratory findings include positive ANA and anti-double-stranded DNA antibody test results.Which of the following cardiac lesions is most likely to be present in this patient? A.Calcific aortic stenosis B.Constrictive pericarditis mn。 E.Rhabdomyoma Ans:D Libman-Sacks endocarditis is an uncommon complication of systemic lupus erythematosus (SLE)that has minimal clinical significance because the small vegetations are unlikely to embolize or cause fumctional flow problems.Calcific aortic stenosis may be seen in older persons with tricuspid valves or it may be a complication of bicuspid valves.Although pericardial effusions are common in SLE they do not cause scarring or constrictive pericarditis.Ischemic cardiomyopathy is unlikely in persons with autoimmune disease who have less
Commotiocordisis a lethal disruption of heart rhythm that occurs as a result of a blow to the area directly over the heart at a critical time during the cycle of a heart beat which results in ventricular fibrillation. Coronary artery disease resulting in inadequate myocardial perfusion is very rare at this age. Endocarditis presents with fever, chills and sweating. Hemosiderosis results from iron overload. Mitral valvular stenosis is a frequent complication of rheumatic heart disease. It presents clinically with signs and symptoms of heart failure such as dyspnea, orthopnea and paroxysmal nocturnal dyspnea, 10. A previously healthy 20 year old man develops heart failure over a period of several days. He is febrile and complains to his friends that he has chest pain, but he does not seek medical attention. He dies and an autopsy is performed. Examination of the heart shows that both ventricles are dilated but otherwise the myocardium appears normal by gross visual inspection. An H&E-stained histologic section shows numerous inflammatory cells in the myocardium, more than 80% lymphocytes, which expand the interstitial spaces between individual myocytes and surround myocytes. Most of the myocytes are structurally intact and appear viable, although scattered individual myocytes are necrotic. The most likely explanation for this finding is A. Acute fungal myocarditis B. Acute myocardial infarction C. Acute rheumatic fever D. Marantic endocarditis E. Viral myocarditis Ans: E Viral myocarditis can cause a mild disease without any symptoms that resolves itself, or it may cause chest pain, heart failure, or sudden death. Definitive diagnosis requires biopsy which shows edema and an inflammatory infiltrate of lymphocytes and macrophages. Focal destruction of myocytes causes myocardial pump failure.Acute fungal myocarditis is very uncommon in individuals with normal immune function.Acute myocardial infarction is not associated with fever or lymphocytic infiltrate of the myocardium.Acute rheumatic fever is rare in modern affluent populations. Marantic endocarditis is due to aseptic valularvegetations that develop in individuals with chronic debilitating illness. 11. A 31-year old woman has had increasing dyspnea for the past week. Physical examination shows temperature of 37.3ºC, pulse 85/min, respirations 20/min, and blood pressure 150/95 mm Hg. There is dullness to percussion over the lung bases. A chest radiograph shows large bilateral pleural effusions and a normal heart size. Laboratory findings include positive ANA and anti-double-stranded DNA antibody test results. Which of the following cardiac lesions is most likely to be present in this patient? A. Calcific aortic stenosis B. Constrictive pericarditis C. Ischemic cardiomyopathy D. Libman-Sacks endocarditis E. Rhabdomyoma Ans: D Libman-Sacks endocarditis is an uncommon complication of systemic lupus erythematosus (SLE)that has minimal clinical significance because the small vegetations are unlikely to embolize or cause functional flow problems.Calcific aortic stenosis may be seen in older persons with tricuspid valves or it may be a complication of bicuspid valves. Although pericardial effusions are common in SLE they do not cause scarring or constrictive pericarditis. Ischemic cardiomyopathy is unlikely in persons with autoimmune disease who have less

atherosclerosis due to the chronic debilitation that occurs with the underlying disease.Rhabdomyoma is a rare cardiac tumor which occurs in children or patients with tuberous sclerosis. 12.A 68 year old diabetic man has become increasingly lethargic and weak for the past 7 months.On physical examination his temperature is3.9C.pulse 70/min,respirations 15/min,and blood pressure 150/90mm Hg. His blood urea nitrogen is elevated.On auscultation.the physician notes a friction rub.There are no other remarkable findings.A representative gross appearance of the heart is shown above.Which of the following is the most likely diagnosis? A.Bacterial pericarditis B.Metastatic carcinoma C.Myocardial infarct D.Uremic pericarditis E.Systemic lupus erythematosus Ans:D This patien has fbrinousor remic pericarditis which frequently and elevated blood levels Bacterial pericardins causes stabbing chest pin whch breathing and may radiate to the neck shoulder or back.There is usually a fever.Metastasis to the heart is very uncommon.When it does occur,it is usually intraparenchymal.Widely metastatic carcinoma presents clinically with cachexia, malaise and weight loss.Myocardial infarct presents acutely with chest pain.Acute MI may be associated with fibrinous pericarditis overlying the area of infarction.It is not diffuse as seen with this patient.Systemic lupus erythematosus may be associated with pericarditis but this is unusual.ANA titer is elevated and the pericarditis with SLE is serous,not fibrinous
atherosclerosis due to the chronic debilitation that occurs with the underlying disease.Rhabdomyoma is a rare cardiac tumor which occurs in children or patients with tuberous sclerosis. 12. A 68 year old diabetic man has become increasingly lethargic and weak for the past 7 months. On physical examination his temperature is 36.9ºC, pulse 70/min, respirations 15/min, and blood pressure 150/90 mm Hg. His blood urea nitrogen is elevated. On auscultation, the physician notes a friction rub. There are no other remarkable findings. A representative gross appearance of the heart is shown above. Which of the following is the most likely diagnosis? A. Bacterial pericarditis B. Metastatic carcinoma C. Myocardial infarct D. Uremic pericarditis E. Systemic lupus erythematosus Ans: D This patient has fibrinous or uremic pericarditis which frequently occurs with renal failure and elevated blood urea nitrogen levels. Bacterial pericarditis causes stabbing chest pain which increases with breathing and may radiate to the neck shoulder or back. There is usually a fever. Metastasis to the heart is very uncommon. When it does occur, it is usually intraparenchymal. Widely metastatic carcinoma presents clinically with cachexia, malaise and weight loss. Myocardial infarct presents acutely with chest pain. Acute MI may be associated with fibrinous pericarditis overlying the area of infarction. It is not diffuse as seen with this patient. Systemic lupus erythematosus may be associated with pericarditis but this is unusual. ANA titer is elevated and the pericarditis with SLE is serous, not fibrinous