Week 18 Quiz 2GIpathology C Elsevier 2005 A-yearod man has compained of"meals for the past decade.remarkable Upper gastrointestinal endoscopy is performed,and an esophageal biopsy specimen is taken from an erythematous area of velvety mucosa just above the gastroes ophageal junction is shown above.Microscopically,the mucosa shows columnar metaplasia with goblet cells.Which of the following MOSI LIKELY produced these findings? A.Achalasia B.Esophageal varices C.Gastroesophageal reflux disease D.Iron deficiency anemia E.Radiation therapy Ans:C Columnar metaplasia of the lower quence of F。12080)n740i y he ac Achalasia fthe lower ES) e the lev of the LES.Varices result from long st Although er is not present.Upper esophageal webbi ng may rareb columnar metaplasia
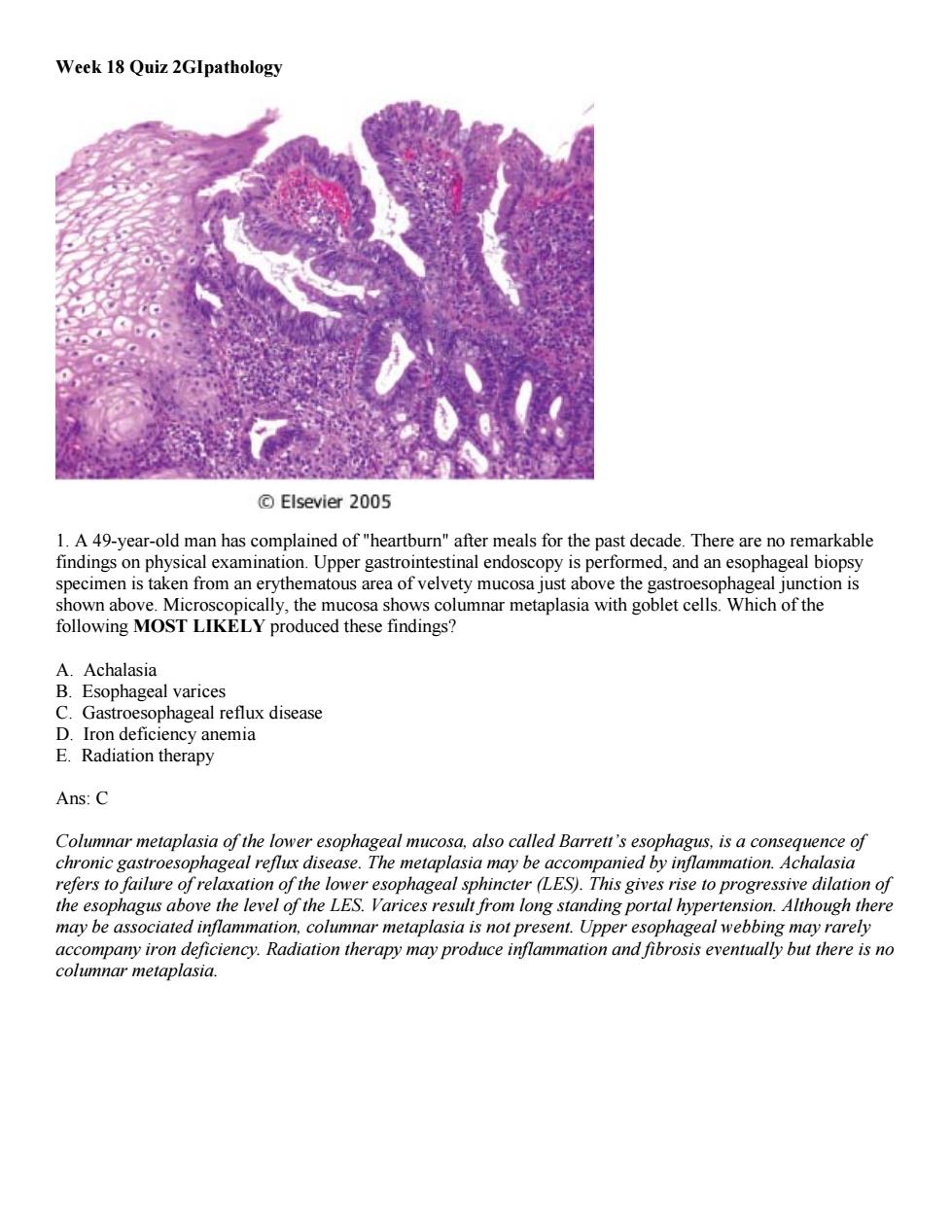
Week 18 Quiz 2GIpathology 1. A 49-year-old man has complained of "heartburn" after meals for the past decade. There are no remarkable findings on physical examination. Upper gastrointestinal endoscopy is performed, and an esophageal biopsy specimen is taken from an erythematous area of velvety mucosa just above the gastroesophageal junction is shown above. Microscopically, the mucosa shows columnar metaplasia with goblet cells. Which of the following MOST LIKELY produced these findings? A. Achalasia B. Esophageal varices C. Gastroesophageal reflux disease D. Iron deficiency anemia E. Radiation therapy Ans: C Columnar metaplasia of the lower esophageal mucosa, also called Barrett’s esophagus, is a consequence of chronic gastroesophageal reflux disease. The metaplasia may be accompanied by inflammation. Achalasia refers to failure of relaxation of the lower esophageal sphincter (LES). This gives rise to progressive dilation of the esophagus above the level of the LES. Varices result from long standing portal hypertension. Although there may be associated inflammation, columnar metaplasia is not present. Upper esophageal webbing may rarely accompany iron deficiency. Radiation therapy may produce inflammation and fibrosis eventually but there is no columnar metaplasia
Elsevier 2005 2.A27-yea-ld man has had for several weeks On physical examination,he is afebrile;there is mild lower abdominal tenderness but no masses,and bowel sounds are present.A stool sample is positive for occult blood.The symptoms subside within I week.Six months later,the abdominal pain recurs with perianal pain.On physical examination,there is now a perirectal fistula.Colonoscopy shows many areas of mucosal edema and ulceration and some areas that appear normal.A biopsy specimen from an ulcerated area is obtained and shows a patchy acute and chronic inflammatory infiltrate,crypt abscesses,and several noncaseating granulomas.Which of the following underlying disease processes BEST EXPLAINS these findings? A.Amebiasis B.Crohn disease C.Sarcoidosis D.Shigellosis E.Ulcerative colitis Ans:B The ileum shows chronic inflamm ation with lymphoid aggregates.The inflam the There is als roenteric oops of smal are more common.extension of fissures into the overlying s in can produce enterocutaneous fistulas.Although the risk of adenocarcinoma is increased in Crohn disease,this complication is less common than the sequelae of inflammation.Amebiasis is characterized by dysentery (severe,ofien bloody diarrhea).Organisms most commonly affect the cecum and ascending colon.The neutrophilic response to the infection creates a flask shaped ulcer with a narrow neck and broad base.Sarcoidosis is characterized by granulomatous inflammation but it most frequently affects the lungs and hilar lymph nodes.Eyes and skin may be affected.Sarcoidosis in the GI tract is uncommon.Fistulas generally do not develop.Shigella infections are most common in the left colon. Shigellosis is a self-limited disease with watery diarrhea that progresses to dysentery in about 50%of patients. It is not associated with granulomatous inflammation.Ulcerative colitis affects the colon.Inflammation is confined to the mucosa.It is not transmural
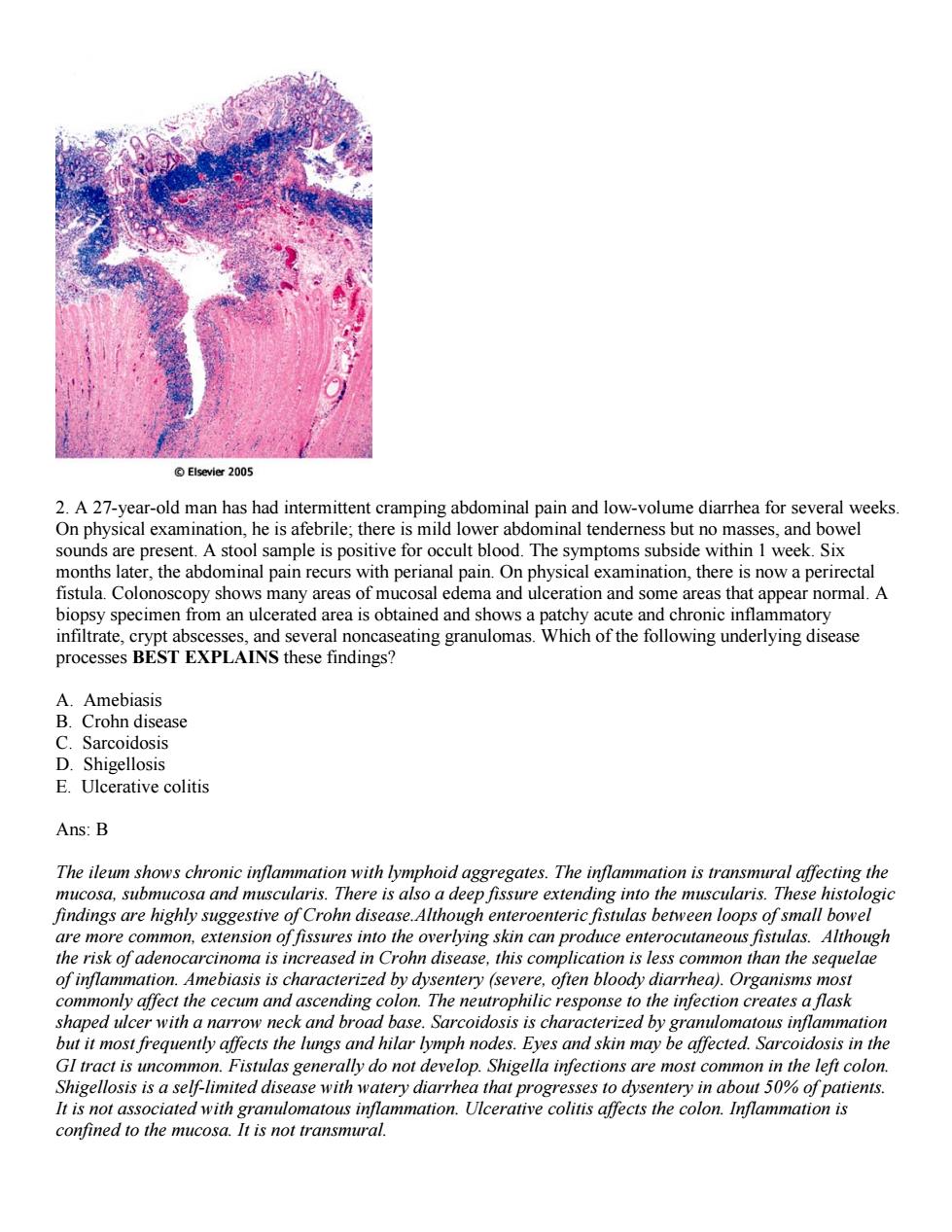
2. A 27-year-old man has had intermittent cramping abdominal pain and low-volume diarrhea for several weeks. On physical examination, he is afebrile; there is mild lower abdominal tenderness but no masses, and bowel sounds are present. A stool sample is positive for occult blood. The symptoms subside within 1 week. Six months later, the abdominal pain recurs with perianal pain. On physical examination, there is now a perirectal fistula. Colonoscopy shows many areas of mucosal edema and ulceration and some areas that appear normal. A biopsy specimen from an ulcerated area is obtained and shows a patchy acute and chronic inflammatory infiltrate, crypt abscesses, and several noncaseating granulomas. Which of the following underlying disease processes BEST EXPLAINS these findings? A. Amebiasis B. Crohn disease C. Sarcoidosis D. Shigellosis E. Ulcerative colitis Ans: B The ileum shows chronic inflammation with lymphoid aggregates. The inflammation is transmural affecting the mucosa, submucosa and muscularis. There is also a deep fissure extending into the muscularis. These histologic findings are highly suggestive of Crohn disease.Although enteroenteric fistulas between loops of small bowel are more common, extension of fissures into the overlying skin can produce enterocutaneous fistulas. Although the risk of adenocarcinoma is increased in Crohn disease, this complication is less common than the sequelae of inflammation. Amebiasis is characterized by dysentery (severe, often bloody diarrhea). Organisms most commonly affect the cecum and ascending colon. The neutrophilic response to the infection creates a flask shaped ulcer with a narrow neck and broad base. Sarcoidosis is characterized by granulomatous inflammation but it most frequently affects the lungs and hilar lymph nodes. Eyes and skin may be affected. Sarcoidosis in the GI tract is uncommon. Fistulas generally do not develop. Shigella infections are most common in the left colon. Shigellosis is a self-limited disease with watery diarrhea that progresses to dysentery in about 50% of patients. It is not associated with granulomatous inflammation. Ulcerative colitis affects the colon. Inflammation is confined to the mucosa. It is not transmural
Elsevier 2005 3.A 53-year-old woman comes to her physician for a routine health maintenance examination.The only abnormal finding is a stool specimen that contains occult blood.Colonoscopy shows a 1.5-cm solitary,rounded, polyp on a05cm stalk at the splensician disc is sho in the fi e below at lo nification.When the phy these findings v e patient. which of the follo B ny more polyps will appe within the next few years Other fa s probably have colonic polyps be curative There is a high probability that you will develop endometrial cancer E.You have inherited one defective copy of the APC gene Ans:C The figure shows a solitary pedunculated adenoma of the colon with no evidence of malignancy.Such a small (<2 cm),solitary polyp is unlikely to harbor malignancy and a search for metastasis is not warranted.Patients with hereditary nonpolyposis colorectal cancer have an increased risk of endometrial cancer and develop colon cancer at a young age.Those who inherit a mutant APC gene usually develop hundreds of polyps at a young age.Therefore this patient does not need genetic testing for a somatic mutation in the APCgene 4 a 62-vear-old man sees his physician because he has had fever and back pain for the past 2 days physical examination shows tenderness of the right costovertebral angle.Laboratory studies show leukocytosis and inal pa a sever n a sto lowngonishe MOSIKELYto have o deveoped E.Pseudomembranous colitis Ans:E
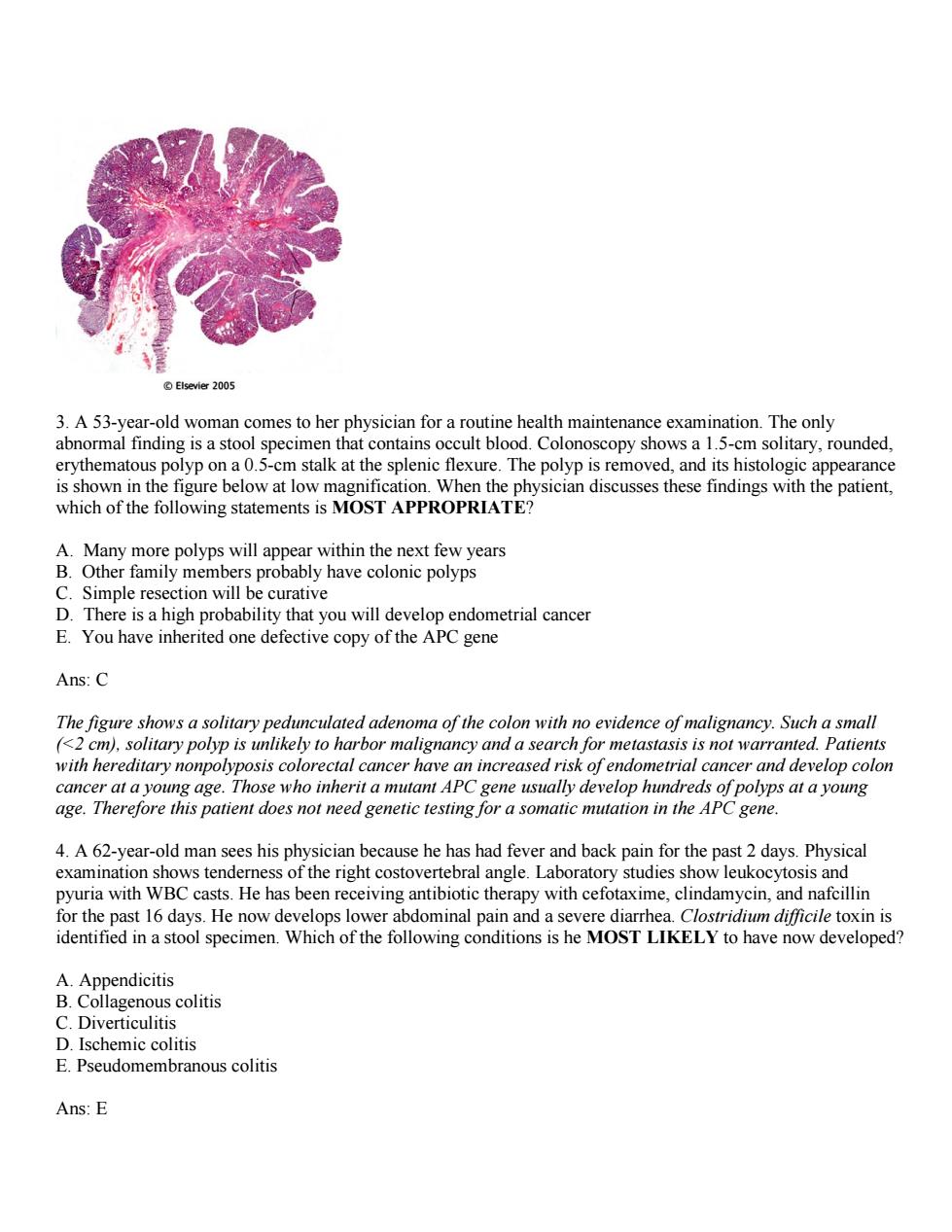
3. A 53-year-old woman comes to her physician for a routine health maintenance examination. The only abnormal finding is a stool specimen that contains occult blood. Colonoscopy shows a 1.5-cm solitary, rounded, erythematous polyp on a 0.5-cm stalk at the splenic flexure. The polyp is removed, and its histologic appearance is shown in the figure below at low magnification. When the physician discusses these findings with the patient, which of the following statements is MOST APPROPRIATE? A. Many more polyps will appear within the next few years B. Other family members probably have colonic polyps C. Simple resection will be curative D. There is a high probability that you will develop endometrial cancer E. You have inherited one defective copy of the APC gene Ans: C The figure shows a solitary pedunculated adenoma of the colon with no evidence of malignancy. Such a small (<2 cm), solitary polyp is unlikely to harbor malignancy and a search for metastasis is not warranted. Patients with hereditary nonpolyposis colorectal cancer have an increased risk of endometrial cancer and develop colon cancer at a young age. Those who inherit a mutant APC gene usually develop hundreds of polyps at a young age. Therefore this patient does not need genetic testing for a somatic mutation in the APC gene. 4. A 62-year-old man sees his physician because he has had fever and back pain for the past 2 days. Physical examination shows tenderness of the right costovertebral angle. Laboratory studies show leukocytosis and pyuria with WBC casts. He has been receiving antibiotic therapy with cefotaxime, clindamycin, and nafcillin for the past 16 days. He now develops lower abdominal pain and a severe diarrhea. Clostridium difficile toxin is identified in a stool specimen. Which of the following conditions is he MOST LIKELY to have now developed? A. Appendicitis B. Collagenous colitis C. Diverticulitis D. Ischemic colitis E. Pseudomembranous colitis Ans: E
wmo of the normo overgrowth eleton,tight junction barrier loss,cytokine release and apoptosis.Fully developed C.difficile-associated colitis is accompanied by the formation ofpseudomembranes made up of inflammatory cells and debris at the sites of mucosal injury.Other organisms sometimes associated with antibiotic associated diarrhea include Salmonella. C.perfringens Type A or Staphylococcus aureus.Appendicitis presents with acute periumbilical pain and is not associated with antibiotic usage.Collagenous colitis presents with chronic non-bloody diarrhea and weight loss Diverticulitis is a complication of the very common condition,diverticulosis.If a diverticulum becomes obstructed,inflamed or ruptures,diverticulitis occurs.Symptoms are non-specific and variable.Severe cases may progress to peritonitis and or abscess formation.Ischemic colitis is caused by inadequate perfusion of the colon.This may be chronic and symptomatic only after large meals.Alternatively,atherosclerotic plaque rupture and/or critical stenosis of the superior mesenteric artery may result in bowel infarction,peritonitis. sepsis and death. 4.A 30-year-old woman sees her physician because she has had diarrhea and fatigue and has noticed a 3-kg weight loss over the past 6 months.On physical examination,she is afebrile and has mild muscle wasting,but her motor strength is normal.Laborator studies show no occult blood.ova.or parasites in the stool.A bior speci en fr the u show above cial diet with no .The patient ispla at following is the MOSTLIKELY hange in die et produces c improvement diagnosis Lymphangiomatosis E.Whipple disease Ans:A The patient has malabsorption that responded to dietary therapy.She probably has gluten sensitivity celiac sprue which is treated by avoidance of dietary gluten.The histologic features are flattening of the mucosa. diffuse and severe atrophy of the villi and chronic inflammation of the lamina propria.There are increased numbers of intraepithelial lymphocytes.Non-caseating granulomas are found in the intestinal wall in Crohn disease.It generally does not respond to diet lacking wheat or rye grain and has a relapsing and remitting course.Diverticulitis affects the colon,not the jejunum.Lymphangiomatosis is a cong nital condition marked se both in the s sie and number of thin-walled lymphatic are abno ole disease Foamy macrophages ac ate in the lamina proprig.They conain the acinnneete. rymawhippelii
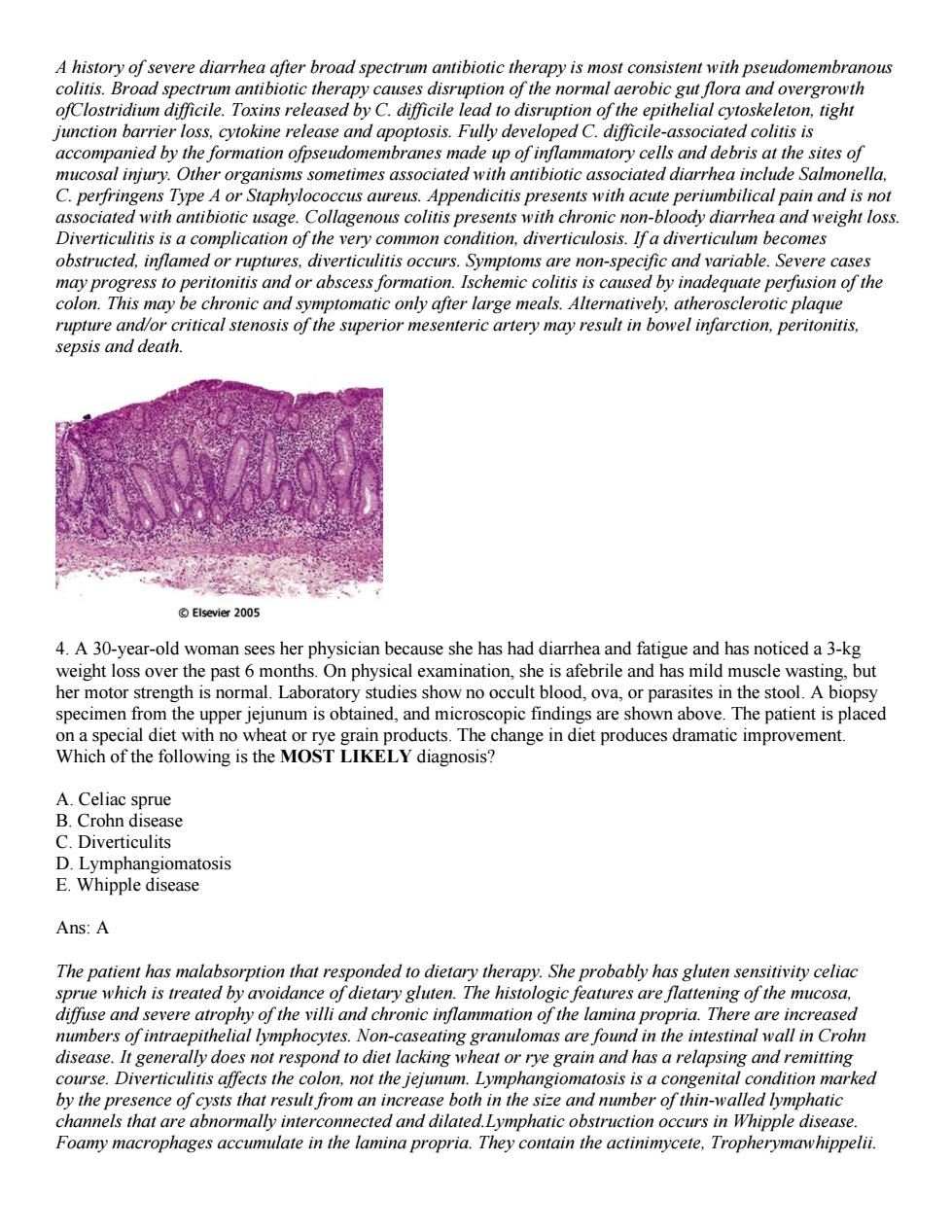
A history of severe diarrhea after broad spectrum antibiotic therapy is most consistent with pseudomembranous colitis. Broad spectrum antibiotic therapy causes disruption of the normal aerobic gut flora and overgrowth ofClostridium difficile. Toxins released by C. difficile lead to disruption of the epithelial cytoskeleton, tight junction barrier loss, cytokine release and apoptosis. Fully developed C. difficile-associated colitis is accompanied by the formation ofpseudomembranes made up of inflammatory cells and debris at the sites of mucosal injury. Other organisms sometimes associated with antibiotic associated diarrhea include Salmonella, C. perfringens Type A or Staphylococcus aureus. Appendicitis presents with acute periumbilical pain and is not associated with antibiotic usage. Collagenous colitis presents with chronic non-bloody diarrhea and weight loss. Diverticulitis is a complication of the very common condition, diverticulosis. If a diverticulum becomes obstructed, inflamed or ruptures, diverticulitis occurs. Symptoms are non-specific and variable. Severe cases may progress to peritonitis and or abscess formation. Ischemic colitis is caused by inadequate perfusion of the colon. This may be chronic and symptomatic only after large meals. Alternatively, atherosclerotic plaque rupture and/or critical stenosis of the superior mesenteric artery may result in bowel infarction, peritonitis, sepsis and death. 4. A 30-year-old woman sees her physician because she has had diarrhea and fatigue and has noticed a 3-kg weight loss over the past 6 months. On physical examination, she is afebrile and has mild muscle wasting, but her motor strength is normal. Laboratory studies show no occult blood, ova, or parasites in the stool. A biopsy specimen from the upper jejunum is obtained, and microscopic findings are shown above. The patient is placed on a special diet with no wheat or rye grain products. The change in diet produces dramatic improvement. Which of the following is the MOST LIKELY diagnosis? A. Celiac sprue B. Crohn disease C. Diverticulits D. Lymphangiomatosis E. Whipple disease Ans: A The patient has malabsorption that responded to dietary therapy. She probably has gluten sensitivity celiac sprue which is treated by avoidance of dietary gluten. The histologic features are flattening of the mucosa, diffuse and severe atrophy of the villi and chronic inflammation of the lamina propria. There are increased numbers of intraepithelial lymphocytes. Non-caseating granulomas are found in the intestinal wall in Crohn disease. It generally does not respond to diet lacking wheat or rye grain and has a relapsing and remitting course. Diverticulitis affects the colon, not the jejunum. Lymphangiomatosis is a congenital condition marked by the presence of cysts that result from an increase both in the size and number of thin-walled lymphatic channels that are abnormally interconnected and dilated.Lymphatic obstruction occurs in Whipple disease. Foamy macrophages accumulate in the lamina propria. They contain the actinimycete, Tropherymawhippelii

©Elsevier2005 6.A 59-year-old man has had nausea and vomiting for several months.He has experienced no hematemesis.On physical examination,there is no abdominal tenderness,and bowel sounds are present.Upper gastrointestinal endoscopy shows erythematous areas of mucosa with thickening of the rugal folds in the gastric antrum.The ymnnrroeWhich f the nac sprue ulcer due to H.pylori infection Ans:C n ulla paiploossp aip pup snoms susiup8.40 1oldd 4alongooo!l disorde cinoma.H toxins which xins released by C cile lead te nsrupton of the epith on is greater tna general prese eliac sprue is gluten sens eeopa ucosa.ay rophy of the prop gene ot affec ch.Shigellosis is bac pro n D species of Shigella us atrophy is a characteristic Celiac sprue
6. A 59-year-old man has had nausea and vomiting for several months. He has experienced no hematemesis. On physical examination, there is no abdominal tenderness, and bowel sounds are present. Upper gastrointestinal endoscopy shows erythematous areas of mucosa with thickening of the rugal folds in the gastric antrum. The microscopic appearance of a gastric biopsy specimen with a Steiner silver stain is shown above. Which of the following is the BEST DIAGNOSIS? A. C. difficileenterocolitis B. Celiac sprue C. Gastric ulcer due to H. pylori infection D. Shigellosis E. Villous atrophy Ans: C Heliocobacter pylori organisms reside in the gastric mucus and are associated with a variety of gastric disorders, including chronic gastritis, peptic ulcers and adenocarcinoma. H. pylori elaborates toxins which injure the epithelium. Broad spectrum antibiotic therapy causes disruption of the normal aerobic gut flora and overgrowth ofClostridium difficile. Toxins released by C. difficile lead to disruption of the epithelial cytoskeleton, tight junction barrier loss, cytokine release and apoptosis. Because the relative role of microbiota in the colon is greater than in the small bowel, C. difficile generally causes colitis rather than enterocolitis. Clinical presentation is with diarrhea. C. difficile does not affect the stomach. Celiac sprue is gluten sensitivity enteropathy. The histologic features are flattening of the intestinal mucosa, diffuse and severe atrophy of the villi and chronic inflammation of the lamina propria. Celiac sprue does generally not affect the stomach.Shigellosis is bacillary dysentery caused by the production of Shiga toxin by several species of Shigella. It is a common cause of epidemic bloody diarrhea world-wide. Villous atrophy is a characteristic histopathologic feature of Celiac sprue