重庆医科大学临床学院教案及讲稿 2004级救 课程名称 心肌病 年级 版、麻醉 授课专业 循环系统 教师 秦俭职称副教授 授课方式※大课示教学时2 题目章节 第九章 教材名称 内科学(全国高等学校教材) 作者主编:叶任高陆再英 出版社人民卫生出版社 版次第6版 教 学 目 掌握心肌病的定义、分类、病理、临床表现、诊断、鉴别诊断及治疗原则。 的 求 教 学 联系病理生理讲述扩张型心肌病和非喉梗阻型心肌病的临床表现及超声心动图的特征性改 难 点 教 学 重 同上。 点 外语 掌握几种不同心肌病的英文名称。 要求 多媒体教学:结合病理讲解。 教学方 法手段 教研 意见 同意通过 教学组长:秦俭 2007年 辅助手段
重庆医科大学临床学院教案及讲稿 课程名称 心肌病 年级 2004 级救 援、麻醉 授课专业 循环系统 教 师 秦 俭 职称 副教授 授课方式 ※大课 示教 学时 2 题目章节 第九章 教材名称 内科学(全国高等学校教材) 作者 主编:叶任高 陆再英 出 版 社 人民卫生出版社 版次 第 6 版 教 学 目 的 要 求 掌握心肌病的定义、分类、病理、临床表现、诊断、鉴别诊断及治疗原则。 教 学 难 点 联系病理生理讲述扩张型心肌病和非喉梗阻型心肌病的临床表现及超声心动图的特征性改 变。 教 学 重 点 同上。 外语 要求 掌握几种不同心肌病的英文名称。 教学方 法手段 教研室 意见 同意通过 教学组长:秦俭 教研室主任:陶小红 2007 年 3 月 18 日 辅助手段 多媒体教学;结合病理讲解
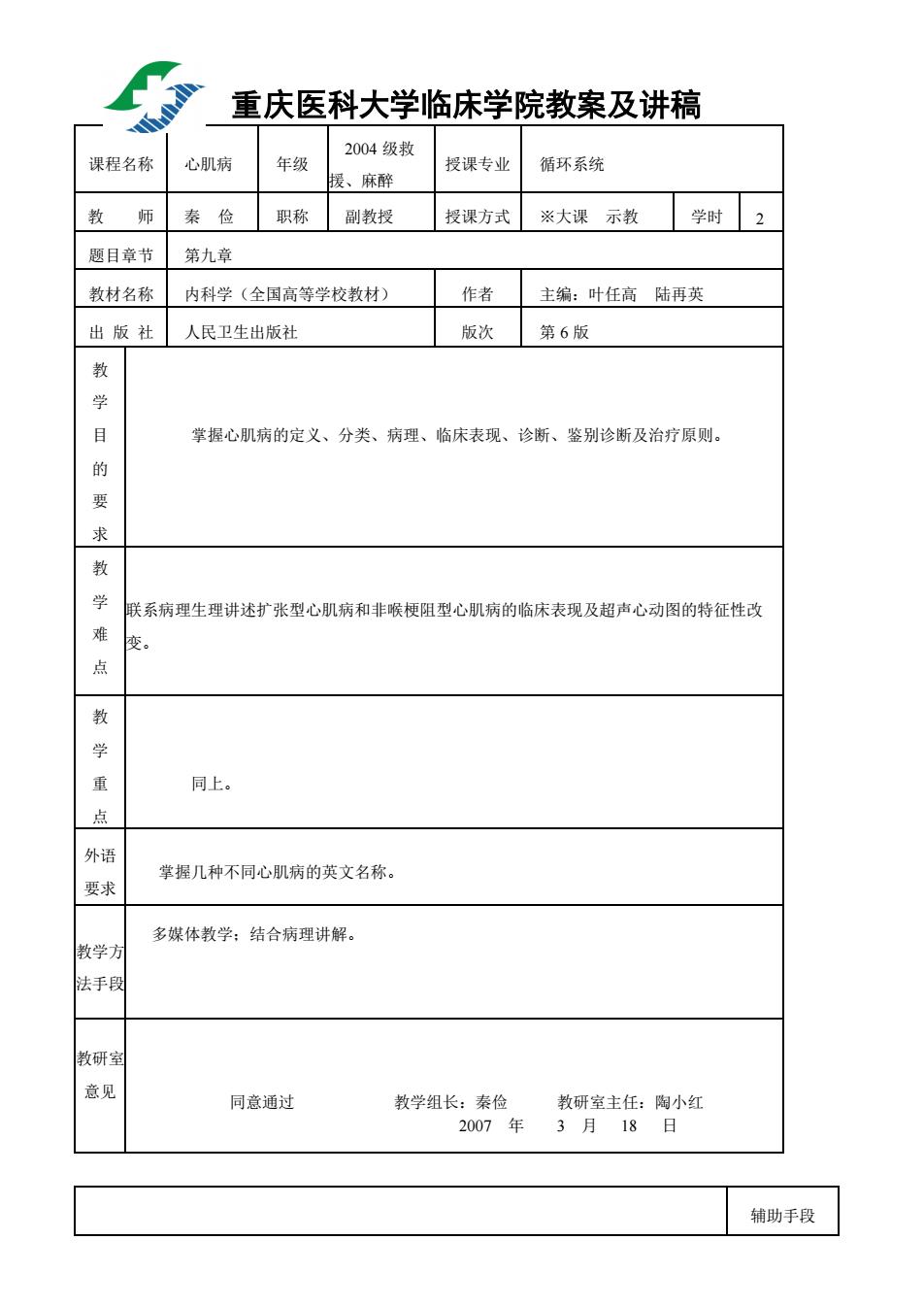
教学内容 时间分配 Cardiomyopathies 1.Introduction 2min They constitute a group of diseases in which the dominant feature is involvement of the heart muscle itself.They are distinctive because they are not the result of pericardial,hypertensive,congenital,valvular,or ischemie diseases.The term Cardiomyopathy"is restricted to diseases solely involving the heart musele that of unknown cause. 2.Classification 3min (1)Idiopathic cardiomyopathies(of unknown cause) Dilated cardiomyopathy (DCM) Hypertrophic cardiomyopathy(HCM) Restrictive cardiomyopathy Arrhythmogenic right ventricular cardiomyopathy Unclassified cardiomyopathies (2)Specific cardiomyopathies (Alcoholic,peripartal,drug-induced and endemic cardiomyopathies) Dilated cardiomyopathy(扩张型心肌病) 73 Normal long axisimage long axis image in DCM 1.Definition DCM isa syndrome characterized by cardiac,impaired systolic function 3min
教学内容 Cardiomyopathies 1. Introduction They constitute a group of diseases in which the dominant feature is involvement of the heart muscle itself. They are distinctive because they are not the result of pericardial, hypertensive, congenital, valvular, or ischemic diseases. The term “ Cardiomyopathy ” is restricted to diseases solely involving the heart muscle that of unknown cause. 2. Classification (1)Idiopathic cardiomyopathies ( of unknown cause): Dilated cardiomyopathy ( DCM ) Hypertrophic cardiomyopathy (HCM) Restrictive cardiomyopathy Arrhythmogenic right ventricular cardiomyopathy Unclassified cardiomyopathies (2) Specific cardiomyopathies (Alcoholic, peripartal , drug-induced and endemic cardiomyopathies ) Dilated cardiomyopathy(扩张型心肌病) Normal long axis image long axis image in DCM 1. Definition DCM is a syndrome characterized by cardiac enlargement , impaired systolic function 时间分配 2min 3min 3min
of one or both ventricles and with or without congestive heart failure.Arrhythmia often occurs.It is most common in middle age and is almost three times more frequent in males than in females.The long-term prognosis is not good. 2.Etiology 2min The cause of disease remains unelear.But there are three possible basic mecha-nisms of damage:familial and genetic factors;viral myocarditis and other cytocoxic insults Immunological abnormalities 3.Pathology 5min Postmortem examination reveals enlargement and dilation of all four chambers;the cardiac valves and coronary arteries are nor-mal,and intracavitary thrombi are common. Histological examination reveals extensive areas of interstitial and perivascular fibrosis,myocardial cell degeneration.Small areas of necrosis are seen on occasion. 4.Clinical manifestations 10min (1)History:A.In the early stage some patients are asymptomatic and later symptoms develop gradually.B.Symptoms of congestive heart failure gradually deteriorate(usually left and right ventricular failures occur simultaneously ).C. Emboli and sudden death may occur.D.All kinds of arrhythmia may occur. (2)Physical examination: A.variable degrees of findings of congestive heart failure; B.variable degrees of cardiac enlargement; C.weakened heart sounds and fast heart rate; D.systolic murmurs due to mitral or tricuspid valvular regurgitation; E.arrhythmia. 5.Laboratory examinations 10min (1)Chest roentgenogram:generalized cardiomegaly and pulmonary vascular redistribution
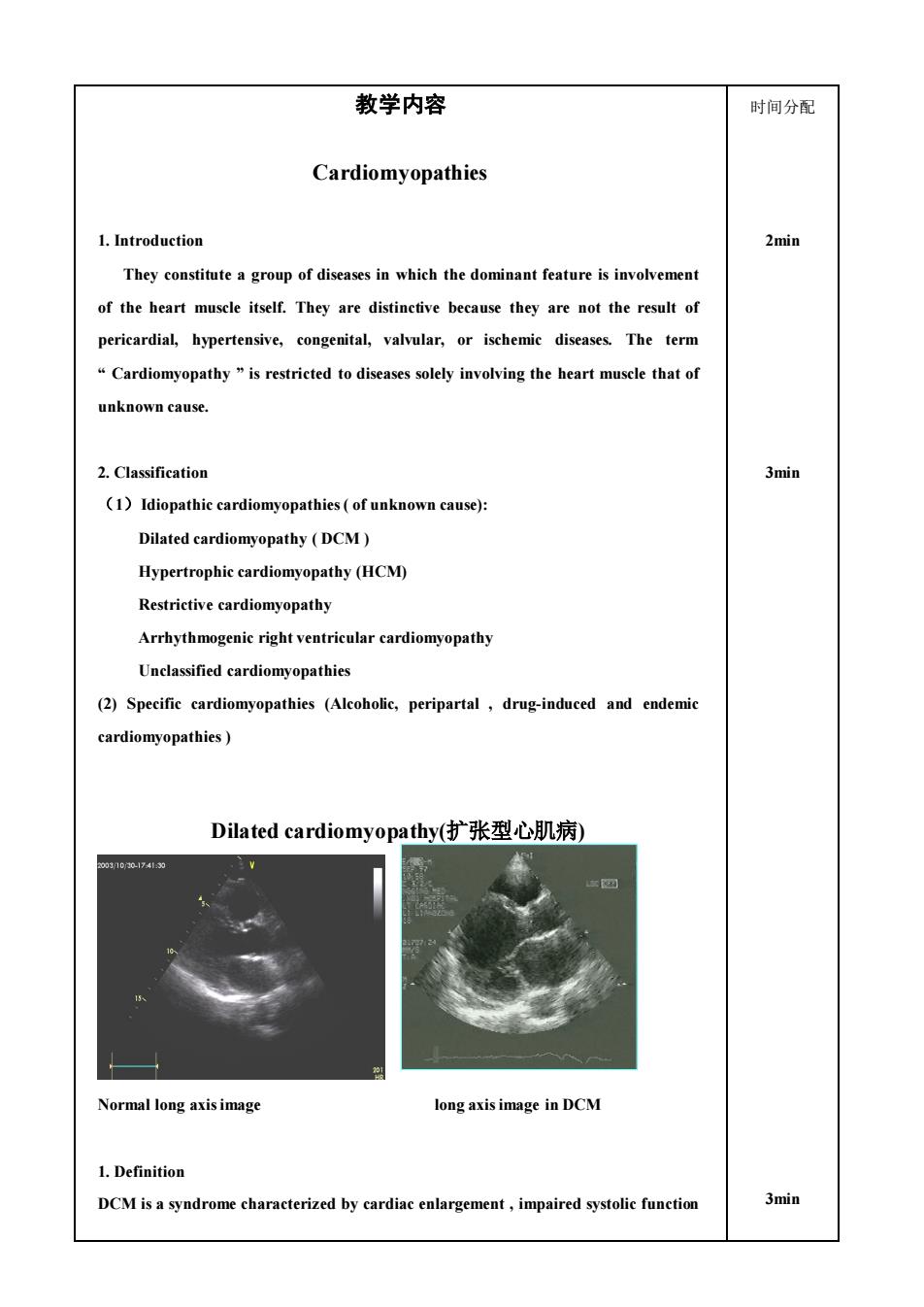
of one or both ventricles and with or without congestive heart failure. Arrhythmia often occurs. It is most common in middle age and is almost three times more frequent in males than in females. The long-term prognosis is not good. 2. Etiology The cause of disease remains unclear. But there are three possible basic mecha-nisms of damage: familial and genetic factors; viral myocarditis and other cytocoxic insults; Immunological abnormalities. 3. Pathology Postmortem examination reveals enlargement and dilation of all four chambers; the cardiac valves and coronary arteries are nor-mal, and intracavitary thrombi are common. Histological examination reveals extensive areas of interstitial and perivascular fibrosis, myocardial cell degeneration. Small areas of necrosis are seen on occasion. 4. Clinical manifestations (1)History: A. In the early stage some patients are asymptomatic and later symptoms develop gradually. B. Symptoms of congestive heart failure gradually deteriorate ( usually left and right ventricular failures occur simultaneously ) . C. Emboli and sudden death may occur. D. All kinds of arrhythmia may occur. (2)Physical examination: A. variable degrees of findings of congestive heart failure; B. variable degrees of cardiac enlargement; C. weakened heart sounds and fast heart rate; D. systolic murmurs due to mitral or tricuspid valvular regurgitation; E. arrhythmia. 5. Laboratory examinations (1)Chest roentgenogram: generalized cardiomegaly and pulmonary vascular redistribution. 2min 5min 10min 10min
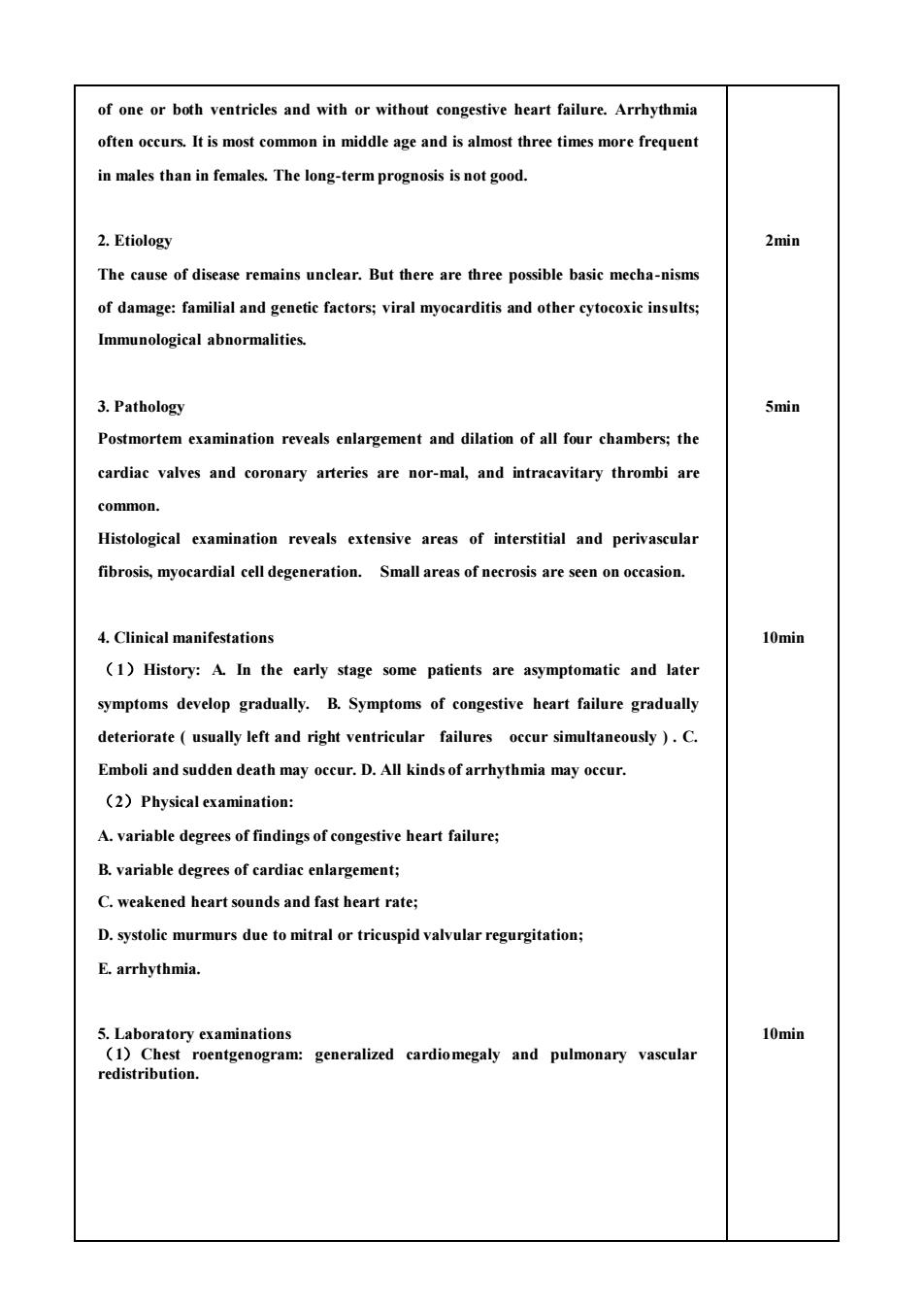
personanda patient with dilated cardiomyopathy,separately (2)Electrocardiography:sinus tachycardia,entire spectrum of atrial and ventricular tachyarrhythmias,intraventricular conduction abnormalities,P-wave change,abnormal Q waves,ST-segment and T wave abnormalities(None of them are special to DCM). (3)Echocardiography:Two-dimensional and Doppler echocardiography are useful in assessing the degree of impairment of left ventricular function and for excluding concomitant valvular or pericardial disease.In addition to examining all four cardiac valves for evidence of structural or functional abnormalities,echocardiography allows evaluation of the size of the ventricular cavity and thickness of the ventricular walls. A.generalized cardiomyogaly(predominant left ventricular enlargement); B.diffuse reduction in wall motion,impaired left ventricular function. Normal four chamber image Four chamber image of DCM (4)Coronary arteriography normal vessels. 2min
Chest roentgenogram from a healthy person and a patient with dilated cardiomyopathy, separately ( 2) Electrocardiography: sinus tachycardia , entire spectrum of atrial and ventricular tachyarrhythmias, intraventricular conduction abnormalities, P- wave change, abnormal Q waves, ST-segment and T wave abnormalities(None of them are special to DCM). (3) Echocardiography: Two-dimensional and Doppler echocardiography are useful in assessing the degree of impairment of left ventricular function and for excluding concomitant valvular or pericardial disease. In addition to examining all four cardiac valves for evidence of structural or functional abnormalities,echocardiography allows evaluation of the size of the ventricular cavity and thickness of the ventricular walls. A. generalized cardiomyogaly (predominant left ventricular enlargement ) ; B. diffuse reduction in wall motion, impaired left ventricular function. Normal four chamber image Four chamber image of DCM (4)Coronary arteriography: normal vessels. 2min
6.Diagnosis and differentiation (1)Clinical manifestations: Unknown cardiac enlargement,congestive hear failure,arrhythmia,without organic murmurs; (2 Echocardiography:Enlargement of four chambers,diffuse reduction in wal motion. Its diagnosis is based on the exclusion of all other known organic heart diseases, including myocarditis,rhematic heart disease,coronary heart disease,hyperten-sive heart disease,chronic pulmonary heart disease and congenital heart diseases. 3min) 7.Management Beeause the cause of idiopathic dilated cardiomyopathy is unknown,specific treatment is impossible.Therefore,treatment is for heart failure (1)Digitalis:easer to overdose on Digitalis. (2)Anticoagulants-recommended. Anticoagulants:Even without controlled clinical trials demonstrating their efficacy,it is recommended in patients with DCM and heart failure; (3)Antiarrhythmias: Although there is no definitive evidence that antiarrhythmatic agents prolong life or prevent sudden death in DCM,it may be appropriate to use them in the treatment of symptomatic arrhythmias.But both efficacy and toxity must be carefully monitored. (4)Cardiac transplantation. 7.Prognosis The long-term prognosis is not good.Greater ventricular enlargement and worse dysfunction tend to correlate with poorer prognosis Patients suffering from DCM usually die of heart failure and/or fatal arrhythmia
6. Diagnosis and differentiation (1) Clinical manifestations: Unknown cardiac enlargement , congestive heart failure, arrhythmia, without organic murmurs; (2) Echocardiography: Enlargement of four chambers, diffuse reduction in wall motion. ※Its diagnosis is based on the exclusion of all other known organic heart diseases , including myocarditis, rhematic heart disease, coronary heart disease, hyperten-sive heart disease, chronic pulmonary heart disease and congenital heart diseases. 7. Management Because the cause of idiopathic dilated cardiomyopathy is unknown, specific treatment is impossible. Therefore, treatment is for heart failure. (1) Digitalis: easer to overdose on Digitalis. (2) Anticoagulants- recommended. Anticoagulants:Even without controlled clinical trials demonstrating their efficacy, it is recommended in patients with DCM and heart failure; (3) Antiarrhythmias: Although there is no definitive evidence that antiarrhythmatic agents prolong life or prevent sudden death in DCM,it may be appropriate to use them in the treatment of symptomatic arrhythmias . But both efficacy and toxity must be carefully monitored. (4) Cardiac transplantation. 7. Prognosis The long-term prognosis is not good. Greater ventricular enlargement and worse dysfunction tend to correlate with poorer prognosis. Patients suffering from DCM usually die of heart failure and/or fatal arrhythmia. 3min) 1min
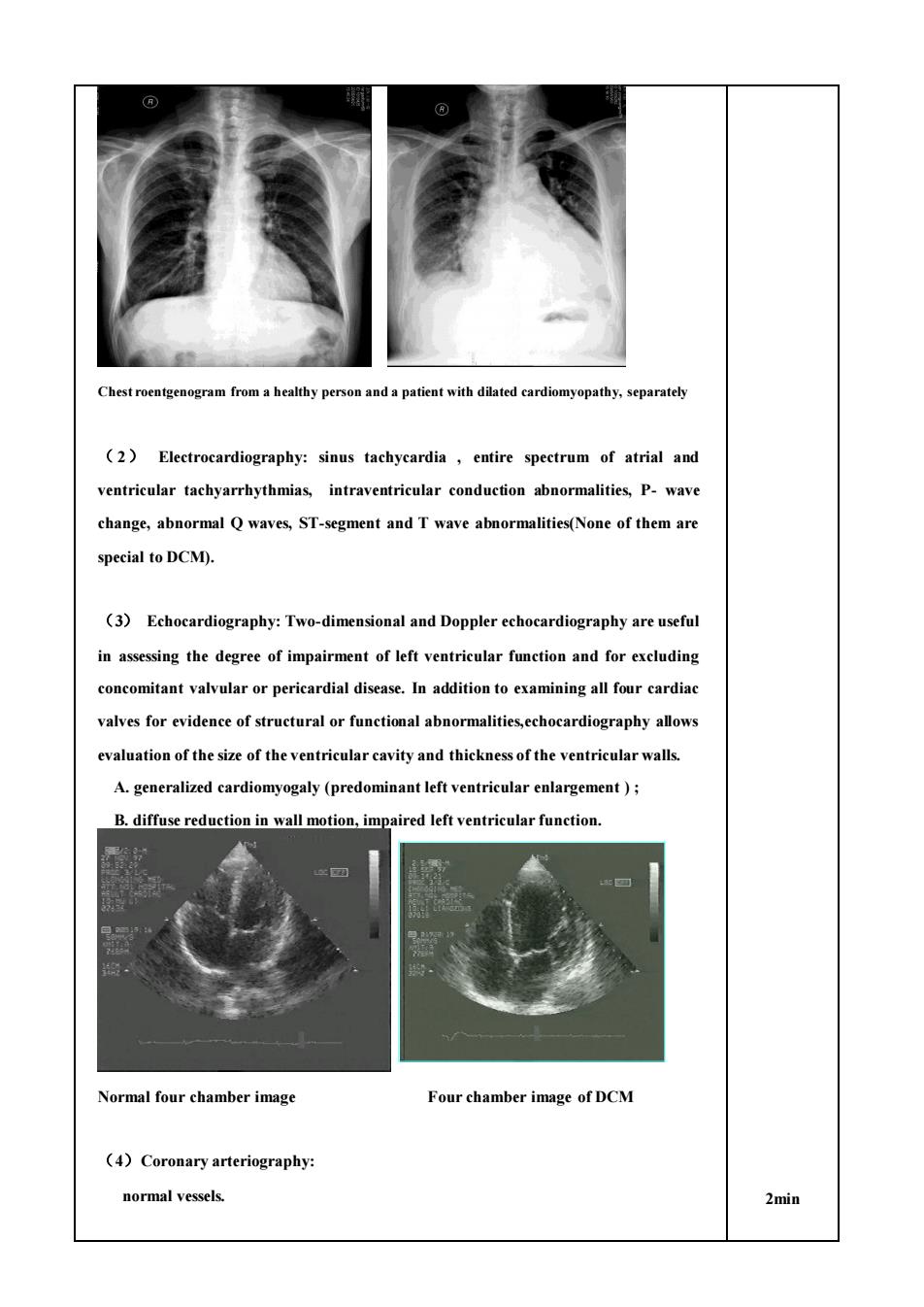
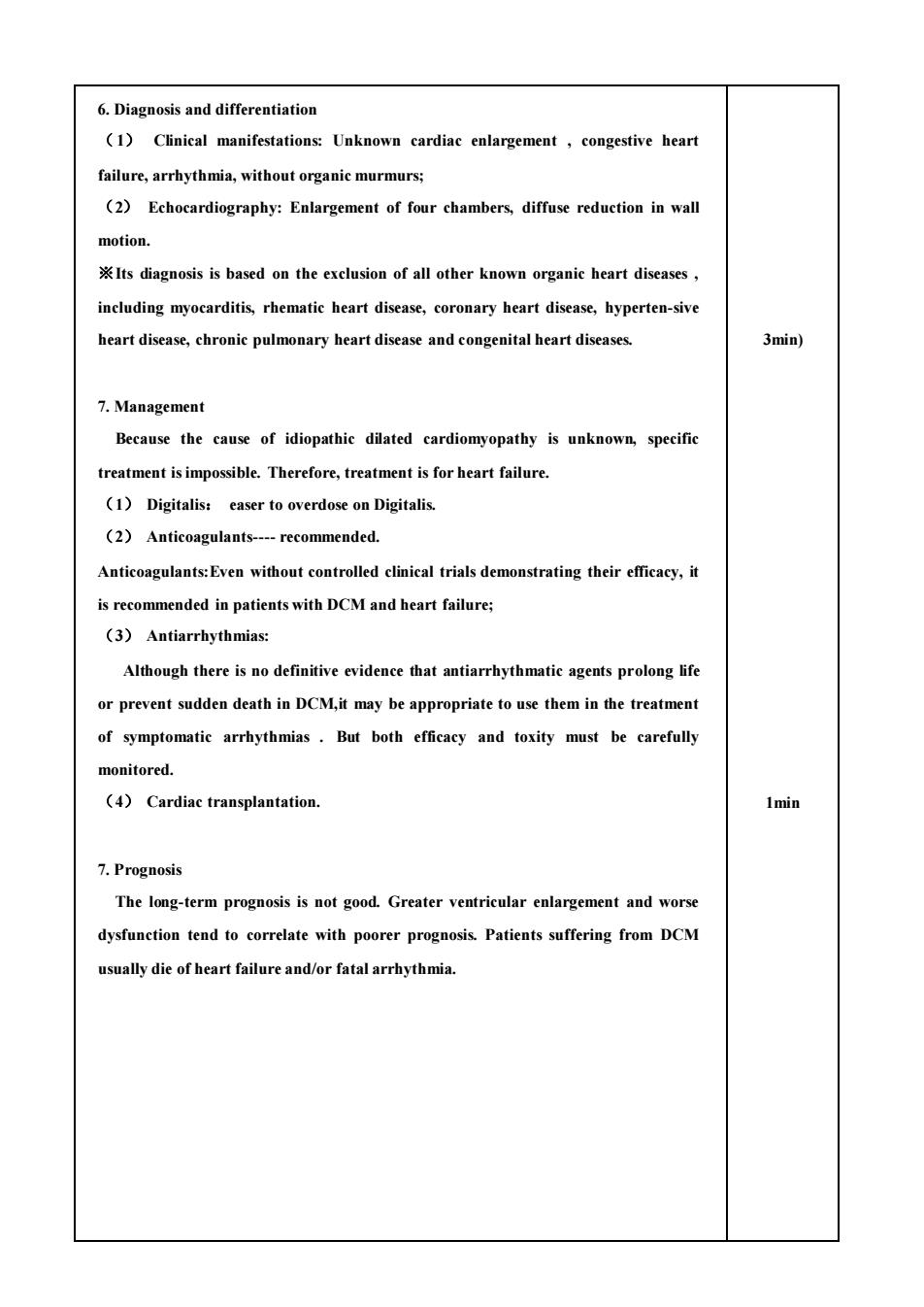
Hypertrophic cardiomyopathy(肥厚型心肌病 室流出道 肥不性心肌病解制结构示意图 non-obstructive hypertrophic obstructive hypertrophic 1min cardiomyopathy cardiomyopathy 1.Introduction HCM was characterized by inappropiate myocardial hypertrophy that occurs in the absence of obvious cause for the hypertrophy (such as aortic stenosis or systemic hypertension).Its most characteristic pathophysiological abnormality is diastolic dusfunction.Thus HCM is characterized by abnormal stiffness of the ventricle with the resultant 2min impaired ventricular filling which leads to its symptoms. 2.Classification According to whether the patient has or has not narrowed left ventricular outflow tract,HCM is classified as obstructive hypertrophic cardiomyopathy and non-obstructive hypertrophic cardiomyopathy. Obstructive hypertrophic cardiomyopathy was referred as idiopathic 1min hypertrophic subaortic stenosis IHSS). 3.Etiology The cause of myocardial hypertrophy in HCM remains unknown.The disease appears to be genetically transmitted In about half the patients. Suggested causes include:genetics;abnormal myocardial calcium kinetics; abnormal sympathetic stimulation;abnormally thickened intramural coronary arteries;subendocardial ischemia and structural abnormality
Hypertrophic cardiomyopathy (肥厚型心肌病) non-obstructive hypertrophic obstructive hypertrophic cardiomyopathy cardiomyopathy 1. Introduction HCM was characterized by inappropiate myocardial hypertrophy that occurs in the absence of obvious cause for the hypertrophy ( such as aortic stenosis or systemic hypertension). Its most characteristic pathophysiological abnormality is diastolic dusfunction. Thus HCM is characterized by abnormal stiffness of the ventricle with the resultant impaired ventricular filling which leads to its symptoms. 2. Classification According to whether the patient has or has not narrowed left ventricular outflow tract, HCM is classified as obstructive hypertrophic cardiomyopathy and non-obstructive hypertrophic cardiomyopathy. Obstructive hypertrophic cardiomyopathy was referred as idiopathic hypertrophic subaortic stenosis ( IHSS ). 3. Etiology The cause of myocardial hypertrophy in HCM remains unknown. The disease appears to be genetically transmitted In about half the patients. Suggested causes include: genetics ; abnormal myocardial calcium kinetics; abnormal sympathetic stimulation;abnormally thickened intramural coronary arteries; subendocardial ischemia and structural abnormality 1min 2min 1min PWLV 左 室 后 壁 左 室 后 壁 PWLV 左 室 流 出 道(LVOT) 左 室 流 出 道(LVOT)
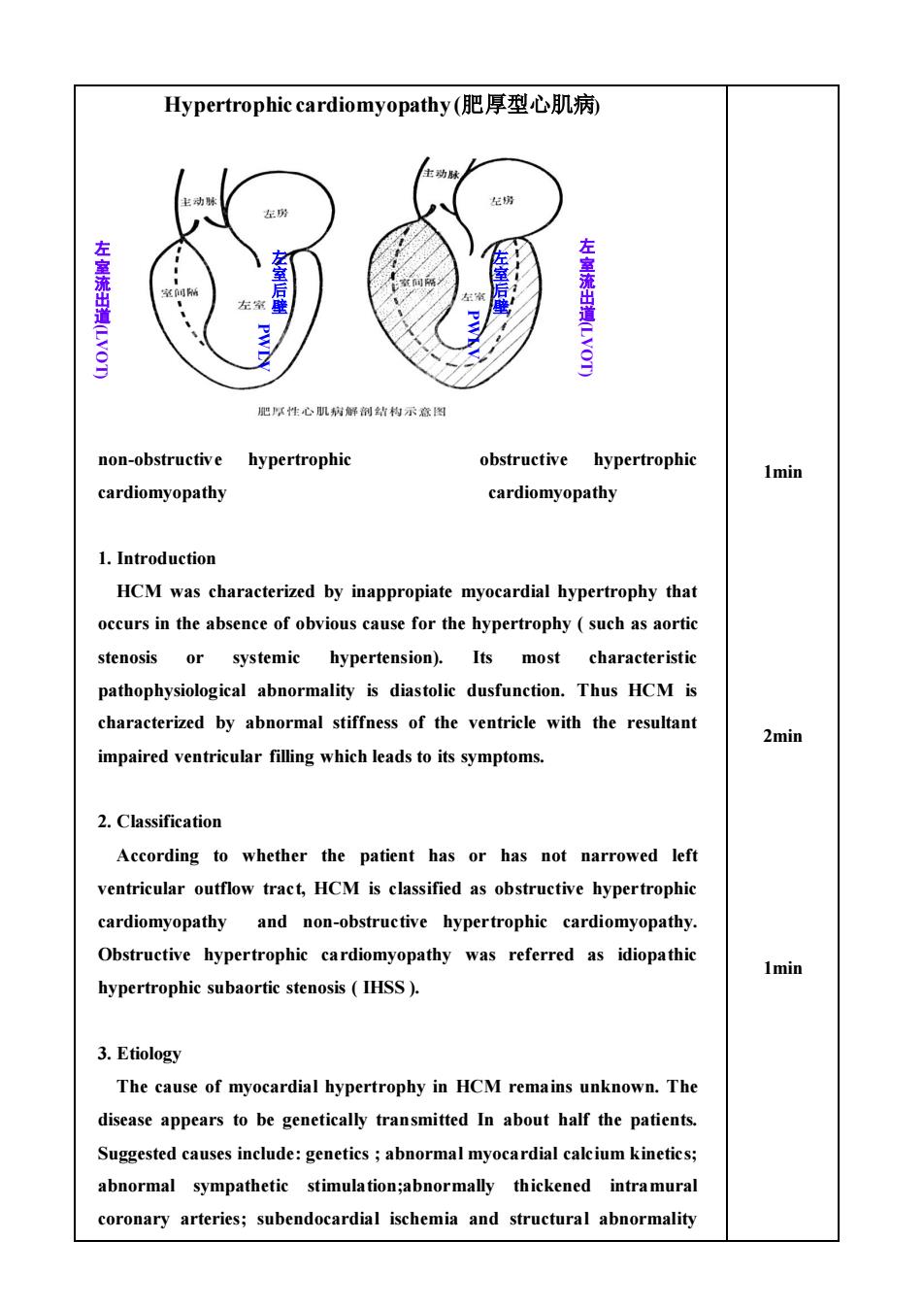
including a catenoid configuration of the septum. 8min 4.Pathology (1)Macroscopic examination typically discloses a marked a marked increase in myocardial mass and small ventricular cavities.The left ventricle is usually more involved with the hypertrophic process than is the right.A typical feature found in most patients with HCM is disproportionate involvement of the interventricular septum and anterolateral wall(Asymmetric septal hypertrophy,ASH) (2)Microscopic findings in HCM are distinctive,with myocardial hypertrophy and gross disorganization of the muscle bundles resulting in a characteristic whorled pattern. Early systole: septal hypertrophy,narrowed outflow tract,rapid ejection velocity, Venturi forces,SAM,obstruction to outflow tract. Midsystole. SAM-septal contact is well established. Latesystole: Volume of flow into outflow tract and aorta is much less 8min 5.Clinical Manifestations (1)Symptoms:The clinical picture varies considerably,ranging from asympto-matic patients to incapacitating symptoms.A general relationship exists between the extent of hypertrophy and the severity of symptoms Symptoms include dyspnea,angina pectoris,fatigue,presyncope and syncope,palpitation,dizziness and sudden death.Exertion tends to
including a catenoid configuration of the septum. 4. Pathology (1) Macroscopic examination typically discloses a marked a marked increase in myocardial mass and small ventricular cavities. The left ventricle is usually more involved with the hypertrophic process than is the right. A typical feature found in most patients with HCM is disproportionate involvement of the interventricular septum and anterolateral wall ( Asymmetric septal hypertrophy, ASH ). (2) Microscopic findings in HCM are distinctive, with myocardial hypertrophy and gross disorganization of the muscle bundles resulting in a characteristic whorled pattern. Early systole: septal hypertrophy,narrowed outflow tract,rapid ejection velocity , Venturi forces ,SAM ,obstruction to outflow tract. Midsystole: SAM-septal contact is well established. Latesystole: Volume of flow into outflow tract and aorta is much less. 5. Clinical Manifestations (1) Symptoms: The clinical picture varies considerably, ranging from asympto-matic patients to incapacitating symptoms. A general relationship exists between the extent of hypertrophy and the severity of symptoms. Symptoms include dyspnea, angina pectoris, fatigue, presyncope and syncope, palpitation, dizziness and sudden death. Exertion tends to 8min 8min
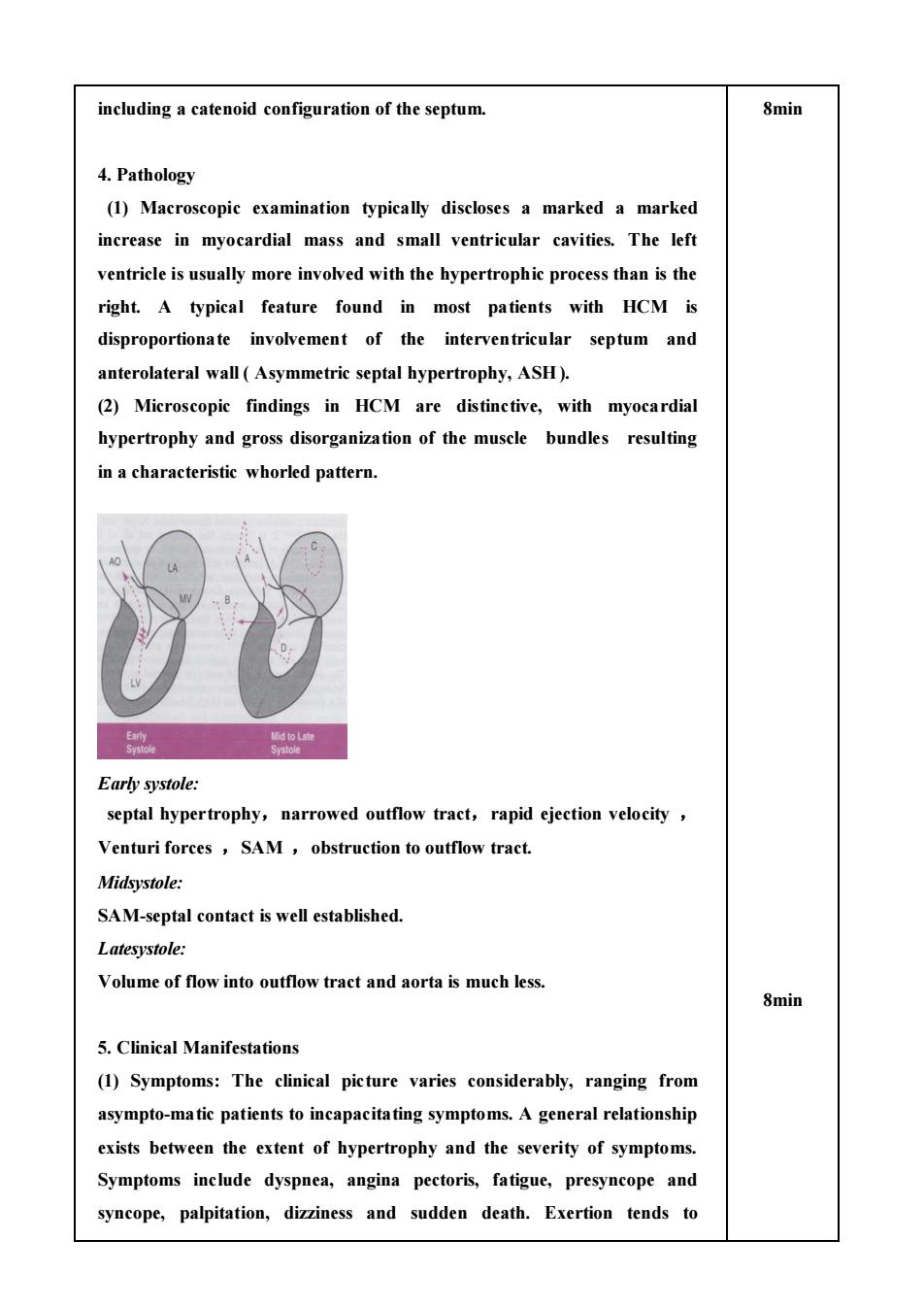
exacerbate many of the symptoms The most common symptom is dyspnea which occurs in up to 90 per cent of symptomatic patients:Hypertrophy,Diastolic dysfunctionImpaired ventricular filling Elevated left ventricular diastolic pressure Elevated atrial and pulmonary venous pressure;Proposed causes of angina pectoris: Inereased muscle mass,inadequate capillary density,elevated diastolic filling pressure,abnormal intramural coronary arteries,enhanced myocardial oxygen demand increased wall stress )Presyncope and syncope may result from inadequate cardiac output with exertion or from cardiac arrhythmias.Presyn-cope and syncope identify patients at increased risk of sudden death. (2)Physical examination:This may be normal in asymptomatic patients without gradients.Findings are usually prominent in patients with a left ventricular outflow tract pressure gradient. Inspection and palpitation:apical precordial impulse. Auscultation:SM in L3-4. 10min 6.Laboratory examinations (1)Electrocardiogram:The most common abnormalities are ST-segment and T-wave abnormalities,followed by evidence of left ventricular hypertrophy,with QRS complexes that are tallest in the midprecordial leads.Giant negative T waves in the midprecordial leads are also characteristic;The Q-wave abnormalities often involve the inferior and/or precordial leads.Ventricular arrhythmias,supraventricular tachycardia, atrial fibrillation may be found. ST-segment and T-wave abnormalities; left ventricular hypertrophy; giant negative T waves in the midprecordial leads; (2)Chest roentegenogram:The cardiac silhouette may range from normal to markedly increased. (3)Echocardiography:Because echocardiography combines the attributes of high resolution and no known risk,it has been widely utilized in the evaluation of HCM.The echocardiogram is of value in identifying and qualifying morphological features,functional aspects and hemodynamic findings
exacerbate many of the symptoms. The most common symptom is dyspnea which occurs in up to 90 per cent of symptomatic patients: Hypertrophy , Diastolic dysfunction → Impaired ventricular filling Elevated left ventricular diastolic pressure Elevated atrial and pulmonary venous pressure;Proposed causes of angina pectoris: Increased muscle mass, inadequate capillary density, elevated diastolic filling pressure, abnormal intramural coronary arteries, enhanced myocardial oxygen demand ( increased wall stress );Presyncope and syncope may result from inadequate cardiac output with exertion or from cardiac arrhythmias. Presyn-cope and syncope identify patients at increased risk of sudden death. (2) Physical examination: This may be normal in asymptomatic patients without gradients. Findings are usually prominent in patients with a left ventricular outflow tract pressure gradient. Inspection and palpitation: apical precordial impulse. Auscultation: SM in L3-4. 6. Laboratory examinations (1) Electrocardiogram: The most common abnormalities are ST- segment and T- wave abnormalities, followed by evidence of left ventricular hypertrophy, with QRS complexes that are tallest in the midprecordial leads. Giant negative T waves in the midprecordial leads are also characteristic; The Q- wave abnormalities often involve the inferior and/or precordial leads. Ventricular arrhythmias, supraventricular tachycardia, atrial fibrillation may be found. ◇ST-segment and T- wave abnormalities; ◇left ventricular hypertrophy; ◇giant negative T waves in the midprecordial leads; (2) Chest roentegenogram: The cardiac silhouette may range from normal to markedly increased. (3) Echocardiography: Because echocardiography combines the attributes of high resolution and no known risk, it has been widely utilized in the evaluation of HCM. The echocardiogram is of value in identifying and qualifying morphological features, functional aspects and hemodynamic findings. 10min

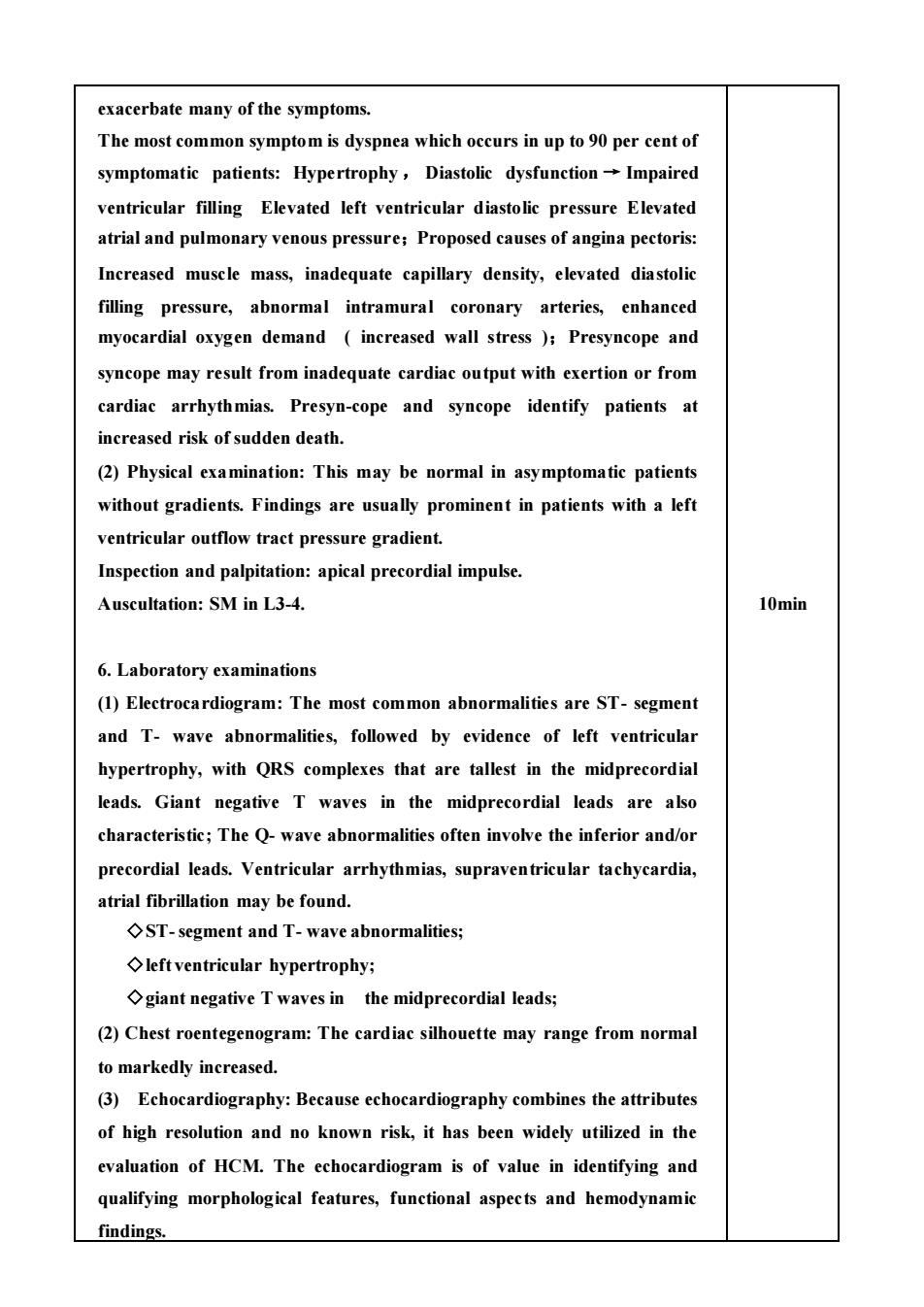
Because echocardiography combines the attributes of high resolution and no known risk,it has been widely utilized in the evaluation of HCM The cardinal echocardiographic feature is left ventricular hypertrophy. The time-honored eriterion for the diagnosis of ASH is the finding of a thickened septum that is at least 1.3 times the thickness of the posterior Normal long axis image Long axis image of HCM A second echocardiographic feature often found in HCM is narrowing of the left ventricular outflow tract which is formed by the interventricular septum anteriorly and the anterior leaflet of the mitral valve posteriorly When HCM is associated with a pressure gradient,there is abnormal systolic anterior motion(SAM of the anterior leaflet. 8min 7.Management (1)Goal:Direct toward alleviation of symptoms,prevention of complications and reduction in the risk of death. (2)Beta-adrenoceptor blockers:These drugs are the mainstay of medical therapy.With their use,angina,dyspnea,and presyncope may all be improved.It may prevent the increase in outflow obstruction that accompanies exercise and decrease the determinants of myocardial oxygen consumption. (3)Calcium antagonists:Both the hypercontractile systolic function and the abnormalities diastolic filling may be related to abnormal calcium kinetics, calcium antagonists may be able to rectify both abnormalities.Verapamil has been the most widely utilized calcium antagonists in this condition.It can decrease the left ventricular outflow gradient.Nifedipine and Diltiazem have also been used in HCM.The combination of a
Because echocardiography combines the attributes of high resolution and no known risk, it has been widely utilized in the evaluation of HCM. The cardinal echocardiographic feature is left ventricular hypertrophy. The time-honored criterion for the diagnosis of ASH is the finding of a thickened septum that is at least 1.3 times the thickness of the posterior wall. Normal long axis image Long axis image of HCM A second echocardiographic feature often found in HCM is narrowing of the left ventricular outflow tract which is formed by the interventricular septum anteriorly and the anterior leaflet of the mitral valve posteriorly. When HCM is associated with a pressure gradient, there is abnormal systolic anterior motion (SAM) of the anterior leaflet. 7. Management (1) Goal: Direct toward alleviation of symptoms, prevention of complications and reduction in the risk of death. (2) Beta-adrenoceptor blockers: These drugs are the mainstay of medical therapy. With their use, angina, dyspnea, and presyncope may all be improved. It may prevent the increase in outflow obstruction that accompanies exercise and decrease the determinants of myocardial oxygen consumption. (3) Calcium antagonists: Both the hypercontractile systolic function and the abnormalities diastolic filling may be related to abnormal calcium kinetics, calcium antagonists may be able to rectify both abnormalities. Verapamil has been the most widely utilized calcium antagonists in this condition. It can decrease the left ventricular outflow gradient. Nifedipine and Diltiazem have also been used in HCM. The combination of a 8min
beta-adrenoceptor blockers and a calcium antagonist may be efficacious in patients responding inadequately to monotherapy. (4)Amiodarone is effective in the treatment of both supraventricular and ventricular tachyarrhythmias in HCM.It improves the prognosis.It may also improve symptoms and exercise capacity. Atrial fibrillation should usually be pharmacologically or electrically converted because of the hemodynamic consequences of the loss of the atrial contribution to ventricular filling in this disorder (5)Other nonsurgical measures: Anticoagulants should be given to patients with chronic atrial fibrillation when no contraindication exists.Strenuous exercise should be avoided because of the risk of sudden death. (6)DDD pacing:Insertion of a dual-chamber DDD pacemaker may be useful in some patients with an outflow gradient and severe symptoms.In high-risk patients or those surviving a cardiac arrest,insertion of an implantable cardioveter-defibrillator should be considered. (7)Infusion of alcohol into a selective catheterized septal artery which leads to intentional infarction of a portion of the interventricular septum is beneficial to a few patients. (8)Surgical treatment:The most popular operation for HCM consists of excising a portion of the hypertrophied septum.Surgery results in long-term improvement in symptoms and exercise capacity in most patients. 2min 8.Prognosis Its progression is slow.In many patients symptoms are absent or mild or remain stable.Adult patients often die of sudden death.Young age(30 yrs)at diagnosis,a family history of HCM with sudden death and fast progression may identify high-risk of the patients
beta-adrenoceptor blockers and a calcium antagonist may be efficacious in patients responding inadequately to monotherapy. (4) Amiodarone is effective in the treatment of both supraventricular and ventricular tachyarrhythmias in HCM. It improves the prognosis. It may also improve symptoms and exercise capacity. Atrial fibrillation should usually be pharmacologically or electrically converted because of the hemodynamic consequences of the loss of the atrial contribution to ventricular filling in this disorder. (5) Other nonsurgical measures: Anticoagulants should be given to patients with chronic atrial fibrillation when no contraindication exists. Strenuous exercise should be avoided because of the risk of sudden death. (6) DDD pacing : Insertion of a dual-chamber DDD pacemaker may be useful in some patients with an outflow gradient and severe symptoms. In high-risk patients or those surviving a cardiac arrest, insertion of an implantable cardioveter-defibrillator should be considered. (7) Infusion of alcohol into a selective catheterized septal artery which leads to intentional infarction of a portion of the interventricular septum is beneficial to a few patients. (8)Surgical treatment: The most popular operation for HCM consists of excising a portion of the hypertrophied septum. Surgery results in long-term improvement in symptoms and exercise capacity in most patients. 8. Prognosis Its progression is slow. In many patients symptoms are absent or mild or remain stable. Adult patients often die of sudden death. Young age (<30 yrs) at diagnosis, a family history of HCM with sudden death and fast progression may identify high-risk of the patients. 2min